Calcitonin gene-related peptide or CGRP for short. That’s the target of most of the new medications developed to treat or prevent migraine attacks, the first medications that were specifically developed for migraine, based on basic science research on migraine pathophysiology.
CGRP monoclonal antibody medications (mabs) are the big ticket new preventive treatments. Previous medications used to prevent migraine were developed for other conditions, and only incidentally found to have some use in migraine treatment (e.g. anti-hypertensives, anti-epileptics, anti-depressants, anti-inflammatories).
But the CGRP mabs are not only at least as effective as other preventives but are more easily tolerated and safer. They can also be effective in people with chronic migraine, medication overuse and those who have not had success with other preventive treatments. And although the CGRP mabs, like all medications, do not work for everyone, there are stories of some people experiencing complete or almost complete remission from migraine attacks, with life-changing results. The rule of thumb for migraine preventives is that they half the number of headache days in about half of people who try them.
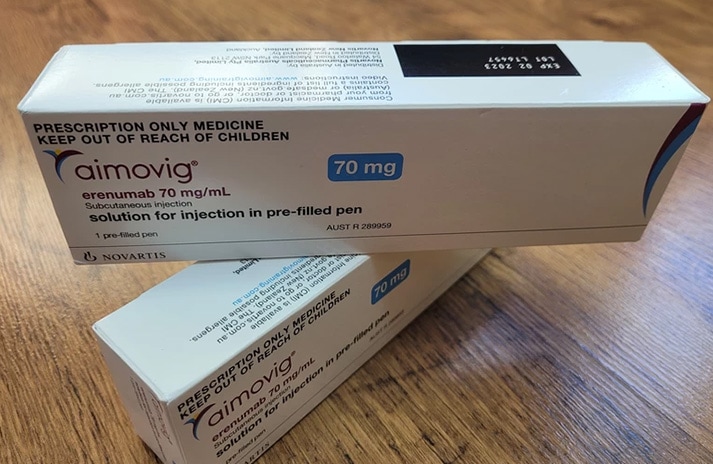
Although there are currently four CGRP mabs used for migraine prevention internationally, as of October 2022 in New Zealand, only three have been approved by Medsafe, only two are available (erenumab/Aimovig and galcanezumab/Emgality) and none are funded. Aimovig is being considered for funding by Pharmac, but probably with a low priority, which in practice means it won’t be funded any time soon, unless the Government increases its spend on medicines. There is not yet an application to Pharmac to fund Emgality, although Migraine Foundation Aotearoa New Zealand is working on one.
I was keen to try a CGRP mab, as I had tried so many preventives before without success. Tricyclic anti-depressants made me too sedated to work, not to mention constipated; and they didn’t work. Beta-blockers made it impossible to walk uphill without feeling like I was about to pass out, not to mention the nightmares; and they didn’t work. Sodium valproate (Epilim) made me fat; and it didn’t work. Pizotifen (Sandomigran) did work, but I was too sleepy to function. Topiramate worked for a while, then stopped working, and gave me an ear-worm of Love is all around (“I feel it in my fingers, I feel it in my toes”) because of the persistent sharp tingling in my hands and feet. Candesartan, verapamil, fluoxetine, lisinopril, melatonin didn’t work. I tried supplements – magnesium, riboflavin, co-enzyme Q10, feverfew, butterbur, Chinese medicine, ayurvedic medicine to no avail.
This litany of failure was depressing, especially as my migraine became chronic, but the mabs gave me hope. They seemed to work well for people who had not benefited from other preventives – maybe even better. I desperately wanted to try one – but was also afraid to. If they didn’t work, then that might be the end of hope, at least for a while. And they were so expensive. At the beginning of 2022, only Aimovig was available in Aotearoa and it cost $678 a month (plus a $50 courier fee, since the only pharmacy that dispensed it was in Auckland, far from where I live).
But my parents nudged me into trying it for six months, offering to pay half the cost since I was only working (in paid work) part time. So at the end of March, I injected my thigh for the first time with a CGRP mab.
April – I’d had an average of 16 headache days a month for the first three months of 2022 and I had 17 in April. The neurologist who’d given me the script for Aimovig had asked about ‘crystal clear’ days, not only headache days. ‘When have you last felt completely free of pain or any migraine symptoms?’ I had to think hard. I often had lingering nausea, even on my headache-free days, frequently had a fuzzy brain and always had fatigue. ‘I can’t remember,’ I had to confess.
May – 17 headache days again. I was starting to get despondent. This wasn’t going to work for me. The only hope I had was from reading a study about ‘late responders’, those who took more than three months before the CGRP mab kicked in. At least I had no side effects.
June – 5 headache days. This felt qualitatively different. I had more energy, my brain was sharper, I didn’t have that blanket-like fatigue. I was struck by how much easier it was to go for a run – some days it felt almost effortless. Near the end of June, my partner went to work in the South Island for three weeks and I became reckless, with no one at home to check my impulses. I wanted to test my limits. Would taking this new drug mean I could stay up beyond 9.30pm and work or write? How much sleep did I really need?
July – 12 headache days, with nine almost in a row that wasn’t pleasant. It turned out I couldn’t skimp on sleep and burn the candle at both ends, just because I was taking Aimovig. It turned out I still needed to keep doing those healthy lifestyle things that help damp down the migraine attacks – regular hours, meals and exercise, good food, yoga, all that jazz. I learnt my lesson. The second half of the month felt promising.
August – 8 headache days. A nasty clump of persistent, non-responsive headache in early August was probably due to an estrogen patch falling off without me noticing. Turns out that Aimovig can’t prevent migraine attacks from fluctuating estrogen levels (at least for me).
September – 10 headache days, but at least three of these were strange headaches I sometimes get at night, which promptly respond to a dose of caffeine and don’t cause any post-headache fatigue or other symptoms. I don’t know if these are proper migraine attacks – if I wake up at night with a migraine, I usually need more than a coffee to set me right and can be wrecked for the rest of the day.
So did Aimovig work for me?
Over the four months that I’d noticed a difference, I had an average of 9 headache days a month, which was pretty close to a decrease of 50%. But even though I still had more headaches than I’d like, they weren’t as severe – I took fewer triptans and non-steroidal anti-inflammatories and when I used them, they worked quickly. This was partly because having fewer attacks meant I was less afraid of medication overuse (which can occur when taking triptans for more than 10 days a month) and didn’t have to ration the triptans, so I took them sooner. The constant fatigue lifted. I had more energy and I could think more clearly – I was more productive at work and work was more enjoyable – I wasn’t battling with brain fog and brain freeze. I felt different – more ‘normal’.
Although my response to Aimovig wasn’t perfect, it gave me the gift of a migraine-free week, not once, but multiple times over the six month trial. A whole week without a migraine attack, nights of sound sleep, undisturbed by pain – that was priceless.
Now we have another CGRP mab in New Zealand, Emgality, which is about half the price of Aimovig and available at any pharmacy. I’m starting on a new trial now, and I finally have an element of hope.
Dr Fiona Imlach, Migraine Foundation Aotearoa New Zealand co-founder
Note: Although CGRP mabs don’t work for everyone, there is anecdotal evidence from overseas that people who don’t find one CGRP mab effective may have a good response to a different one. This is why we want to see all four CGRP mabs available in New Zealand.