Migraine is such a common disease, you’d expect all health professionals would know the best treatments and how to manage acute attacks.
Unfortunately, this often isn’t the case. Migraine is commonly undertreated and mistreated. For example, we often hear from members in our community that they had not been told about or offered triptans for migraine attacks. Triptans are a migraine-specific treatment, unlike generic pain relievers such as aspirin and paracetamol. They’ve been available since the 1990s and are a first-line treatment for migraine attacks. Unfortunately, only two triptans are currently available in New Zealand (there are seven in other parts of the world) and new migraine-specific acute treatments are not yet available here (such as gepants and ditans).
We also hear about inappropriate treatment, where people are given opioids (e.g. codeine, tramadol) rather than triptans. Opioids are not recommended for migraine attacks long-term as they have a significant risk of addiction and exacerbates the problem that occurs during attacks of the stomach being slow to empty (which contributes to nausea and means that other medication isn’t absorbed).
Suboptimal treatment of migraine attacks can lead to chronic migraine and more headache days.
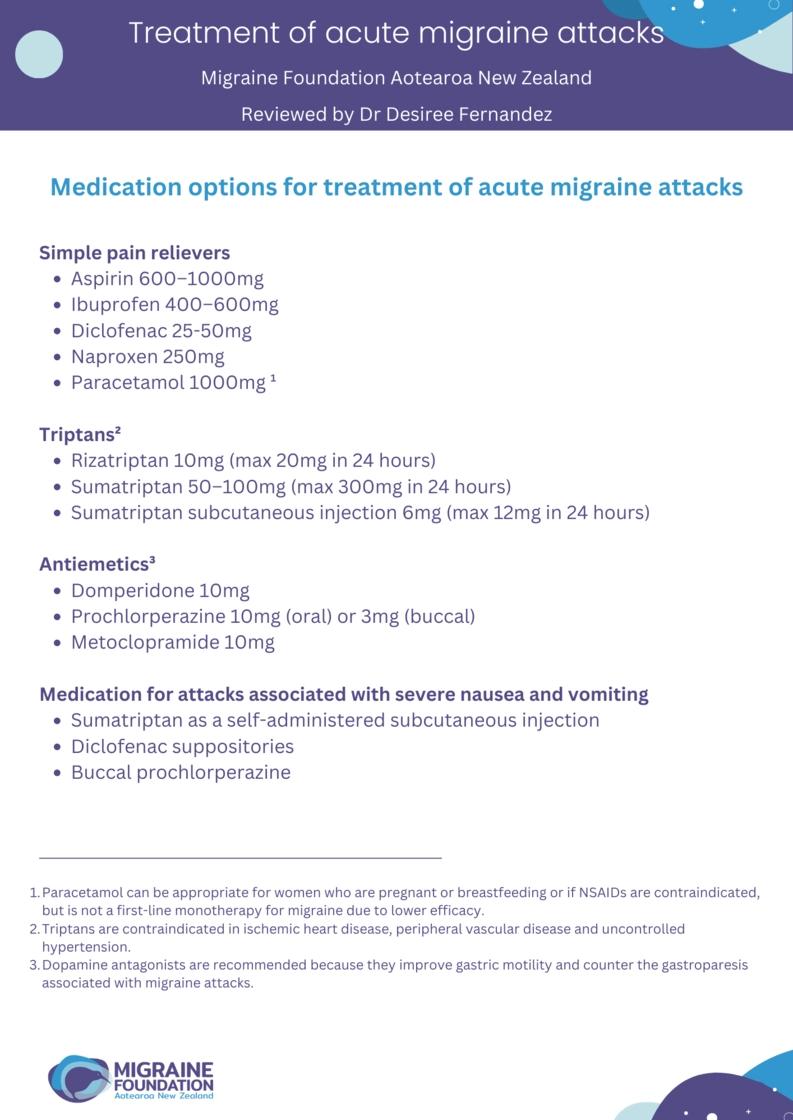
So, what are the recommended treatment options for migraine attacks? Non-steroidal anti-inflammatory drugs (NSAIDs) are often the first point of call, such as aspirin, ibuprofen, naproxen and diclofenac. Triptans are recommended for moderate-severe attacks and when attacks do not respond adequately to NSAIDs (or when NSAIDs can’t be taken for some other reason). Paracetamol often doesn’t work very well for migraine attacks and isn’t considered a first-line therapy on its own, although can be used in combination with NSAIDs.
Here are some evidence-based tips for treating a migraine attack with medication:
- Take medications within 30 minutes of the headache developing. Triptans are not as effective if taken during the aura phase.
- Take medication for nausea (antiemetics) together with pain relievers or triptans to help absorption of medications. Take these even if you don’t feel very nauseated, as the slowed stomach emptying and poor absorption of medication is part of the migraine attack. The specific anti-emetics listed in the table below are the best options as they specifically act to get the stomach moving.
- If treatment is ineffective after two hours, repeating the dose (for that attack) is unlikely to work. Try an alternative or a combination of medications. If the treatment initially worked and the migraine recurs within 48 hours, another dose can be taken.
- Combining an NSAID with a triptan can be successful if you don’t get sufficient relief with either alone.
- If treatment is ineffective after at least two trials, check the medication has been taken optimally before trying a different medication. Was it a high enough dose, taken early within an attack, using an injection or suppository if necessary? Check out the medication options for severe nausea or vomiting on the table.
- Every triptan has a slightly different mechanism of action so if one triptan is not effective, try another one.
An occipital nerve block is another acute treatment option, but this has to be given by a health professional. It involves injection with local anaesthetic of one of the nerves at the back of the skull (the greater occipital nerve). Pain relief can last for several weeks.
Non-medication options include cold therapy, heat therapy, rest, massage, caffeine, ginger, tiger balm or peppermint oil. Nerve stimulation devices can help reduce the pain of an attack through stimulation of the trigeminal nerve, involved in migraine attacks. These can be difficult to find in New Zealand but may be available to purchase online overseas (see more on our non-medication treatment options page)
References
- Ailani J, Burch RC, Robbins MS; Board of Directors of the American Headache Society. The American Headache Society Consensus Statement: Update on integrating new migraine treatments into clinical practice. Headache. 2021 Jul;61(7):1021-1039. doi: 10.1111/head.14153.
- Ashina M, Buse DC, Ashina H, Pozo-Rosich P, Peres MFP, Lee MJ, Terwindt GM, Halker Singh R, Tassorelli C, Do TP, Mitsikostas DD, Dodick DW. Migraine: integrated approaches to clinical management and emerging treatments. Lancet. 2021 Apr 17;397(10283):1505-1518. doi: 10.1016/S0140-6736(20)32342-4.
- British Association for the Study of Headache (BASH). 2019. National Headache Management System for Adults 2019. http://www.bash.org.uk/guidelines/
- Mottershead, J. How to treat: Headache. New Zealand Doctor. 2021 Sep 1: 31-35
- VanderPluym JH, Halker Singh RB, Urtecho M, Morrow AS, Nayfeh T, Torres Roldan VD, Farah MH, Hasan B, Saadi S, Shah S, Abd-Rabu R, Daraz L, Prokop LJ, Murad MH, Wang Z. Acute Treatments for Episodic Migraine in Adults: A Systematic Review and Meta-analysis. JAMA. 2021 Jun 15;325(23):2357-2369. doi: 10.1001/jama.2021.7939.


