Results from the Migraine in Aotearoa New Zealand Survey 2022
There’s a lot in the news about the ongoing changes to our health system but not much is being said about the role and funding of complementary therapies. The focus is on nurses and doctors but there are many other allied health professionals and other practitioners who can be involved in effective migraine treatment. These include occupational therapists, physiotherapists, massage therapists, yoga and Tai Chi instructors, acupuncturists, psychologists and dietitians.
We asked respondents to the Migraine in Aotearoa New Zealand Survey 2022 about whether they’d tried a range of complementary or non-medication approaches to prevent migraine attacks. The majority (58%) were currently using one or more complementary approaches and only 15% had never tried any complementary approach. Even fewer people with chronic migraine (5%) had never tried any of these approaches, compared with 18% of those with episodic migraine.
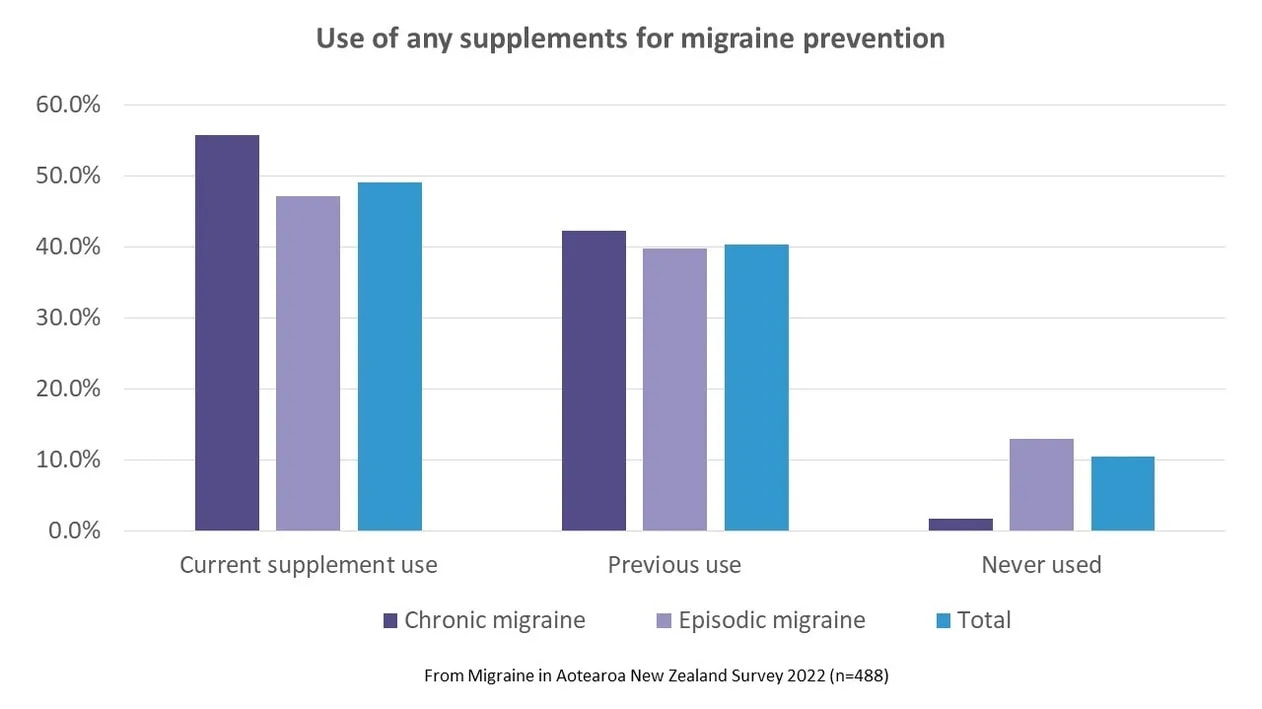
Use of complementary, non-medication approaches was a little higher than use of medications or supplements – about half of respondents were taking one or both of these for migraine prevention. Of those using a complementary approach, more than half (54%) were also taking a prescribed preventive medication and 70% were also using a supplement. From all the respondents who answered these questions, one in five (20%) were currently using prescription medication, supplements and complementary approaches for migraine prevention.
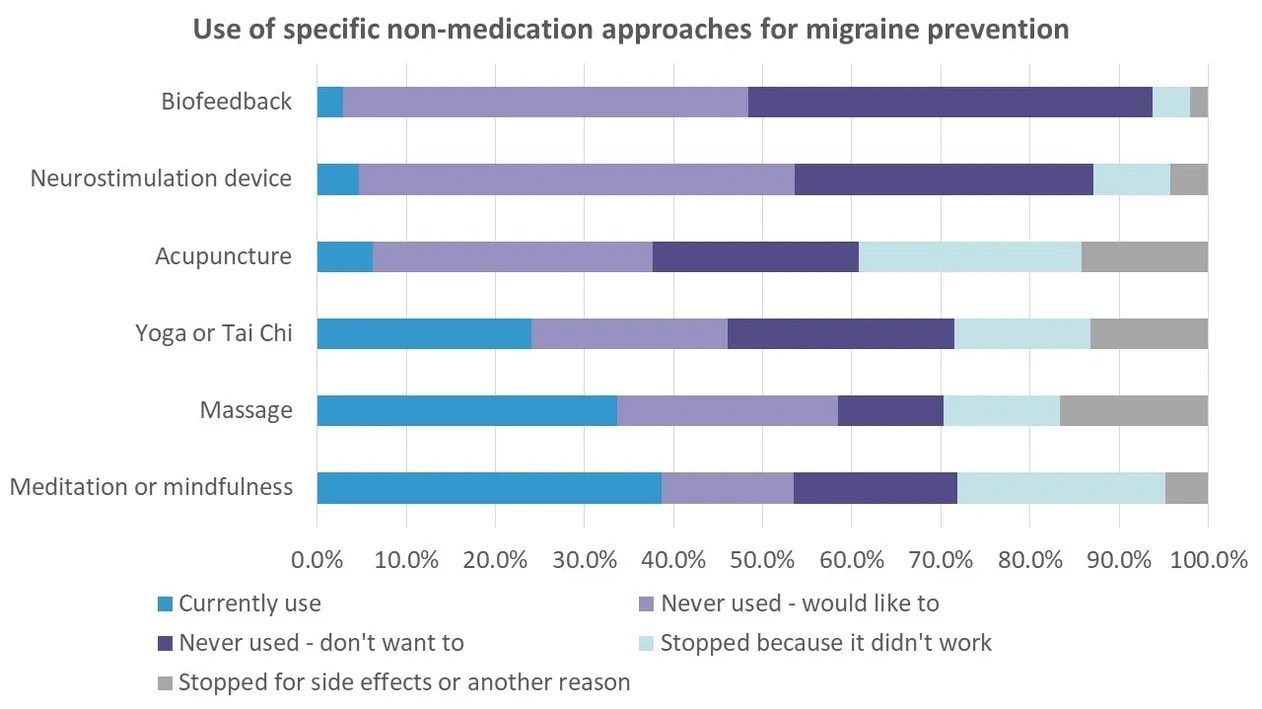
We specifically asked about a variety of non-medication approaches. These were approaches that had at least some evidence for effectiveness in migraine treatment and for which we wanted to know more about how they were being used in New Zealand. These included biofeedback, neurostimulation devices, acupuncture, yoga or Tai Chi, massage therapy and meditation or mindfulness approaches. Other approaches that we didn’t specifically ask about that can help with migraine include relaxation strategies (e.g. progressive muscle relaxation, diaphragmatic breathing, guided imagery), cognitive behavioural therapy for managing pain and/or insomnia, physical therapy, exercise and diet.
Meditation or mindfulness and massage were being used by over a third of respondents (37% and 34% respectively) and yoga or Tai Chi by nearly a quarter (24%). Few people were currently using the other approaches.
Nearly a quarter of respondents had tried and stopped using meditation/mindfulness and acupuncture because it didn’t work. Smaller proportions of people had previously used and stopped the other approaches because of this reason. Stopping because of side effects was rare but people did stop for ‘another reason’. We didn’t specifically ask about the other reasons but in other survey questions, people mentioned cost as a barrier to using complementary therapies.
In some ways, we could consider ourselves fortunate that there are so many different approaches to tackling migraine disease – medications, supplements and a host of complementary therapies. On the other hand, if we want to make the most of all the treatment options, try the latest medicines, the best supplements and all the complementary therapies that might work, we’re likely to be left with a very large hole in our wallets as well as not much time to do anything else.
While debates over increasing resources for the mainstream medical system dominate media and political discussions about health, let’s not forget the importance of non-medical approaches to support health and wellbeing. As a migraine community, maybe we should be asking for better access to and subsidies for complementary therapies that have proven to be beneficial. From this survey, a third to half of respondents had never tried three approaches with a sound evidence base (biofeedback, neurostimulation devices and acupuncture) but would like to. That’s a lot of people that have the potential to benefit. And we need more research into these therapies and whether their use might actually reduce the pressure on the medical system. Now that would be something to get political attention.
Further reading
- Kuruvilla, D. and Wells, R.E. (2019), Evidence-Based Integrative Treatments for Headache. Headache: The Journal of Head and Face Pain, 59: 971-972. https://doi.org/10.1111/head.13555


