Results from the Migraine in Aotearoa New Zealand Survey 2022
Hardly a week goes by without another story about the cracks in our health system. Waiting for weeks for an appointment with a GP. Overflowing emergency departments with no room to unload new patients from the ambulance bay. Elective surgeries were cancelled and deferred. Tests and investigations are delayed, which means further delays in diagnosis and treatment for potentially serious conditions.
From our survey of people with migraine in Aotearoa New Zealand in 2022, there’s no good news about access to health care for migraine, either. We asked respondents if they’d ever wanted to see a health professional for migraine but were unable to. From the 488 people who answered this question, nearly half (48%) said yes, they’d been unable to see a health professional for migraine. This was higher (59%) for people with chronic migraine compared to those with episodic migraine (44%). Chronic migraine is a more severe disease, where people experience headaches on 15 or more days a month, compared to episodic migraine (14 days or less a month). It’s concerning that those who are most likely to need and seek health care, and who are experiencing the greatest amount of disability and pain, have difficulties in accessing health care.
We asked about what type of health professionals people had been unable to see for migraine.
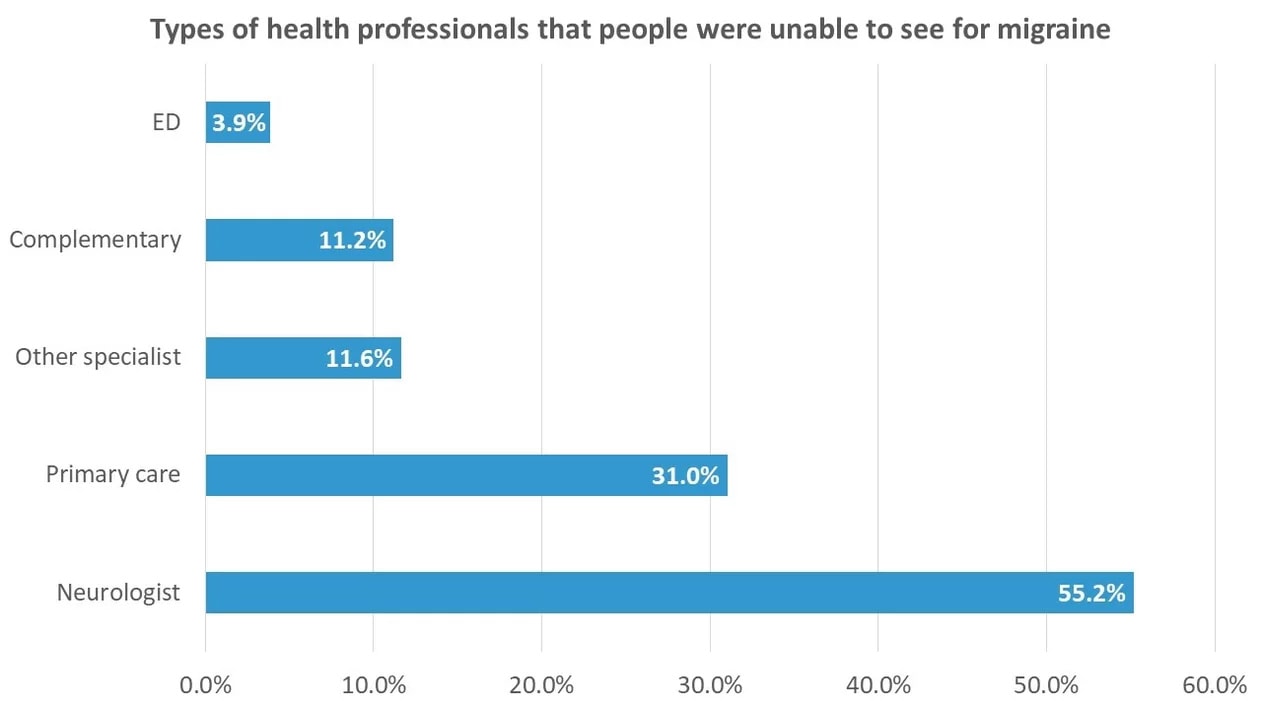
Over half (55%) had been unable to see a neurologist. This aligns with what we commonly hear from the migraine community. Referrals to neurology departments for migraine in the public health system are routinely declined. GPs may even refuse to make a referral. People are being denied access to specialist care because migraine is not considered a serious enough condition to warrant a neurologist’s review and because public neurology services are already overloaded and oversubscribed. The only recourse is often to seek an appointment in private.
Nearly a third (31%) had also been unable to see a GP in primary care. This also aligns with the reports we hear about the creaking health system. Waiting two or three weeks for a GP appointment is no use in the middle of a severe or prolonged migraine attack and although most practices have urgent appointment slots during the day, there’s no guarantee of acquiring one.
We also asked about why people were unable to see a health professional for migraine, using a list of commonly reported barriers to health care used in national surveys. The top three reasons, each given by 43-44% of respondents, were long waiting times, expense and inability to get an appointment.
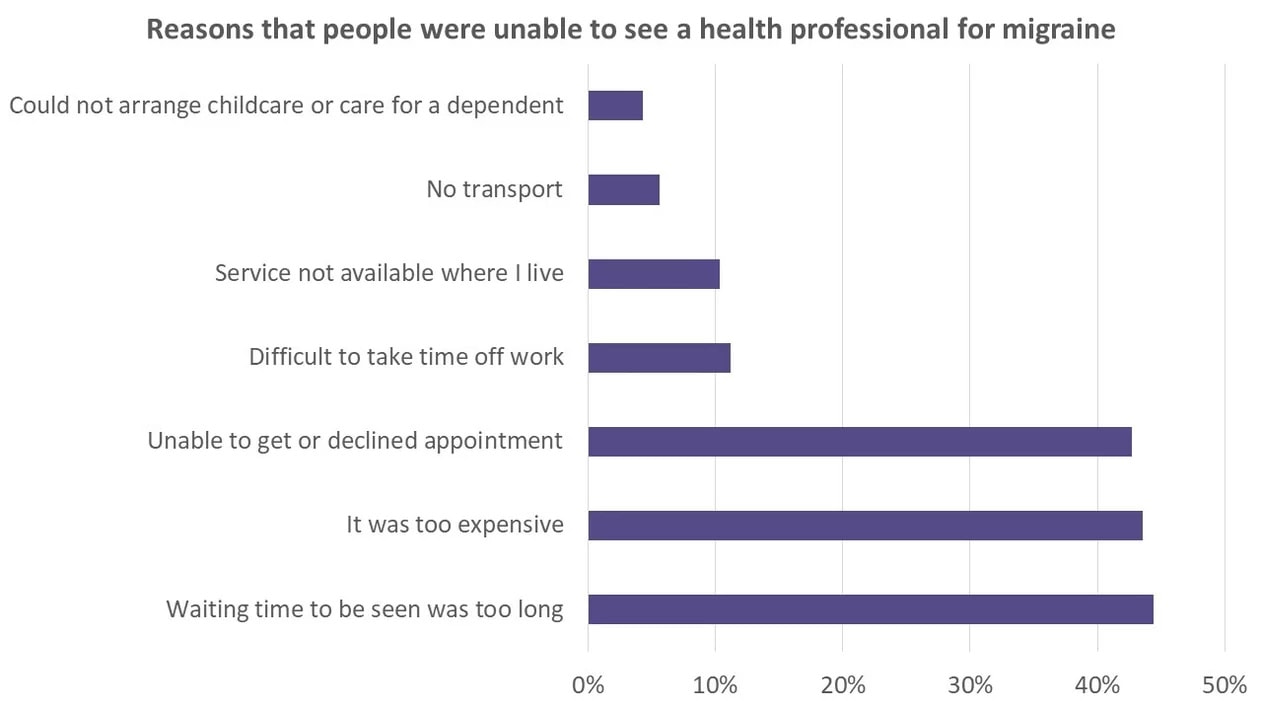
From Migraine in Aotearoa New Zealand survey 2022 (based on respondents who were unable to see a health professional for migraine, n=232)
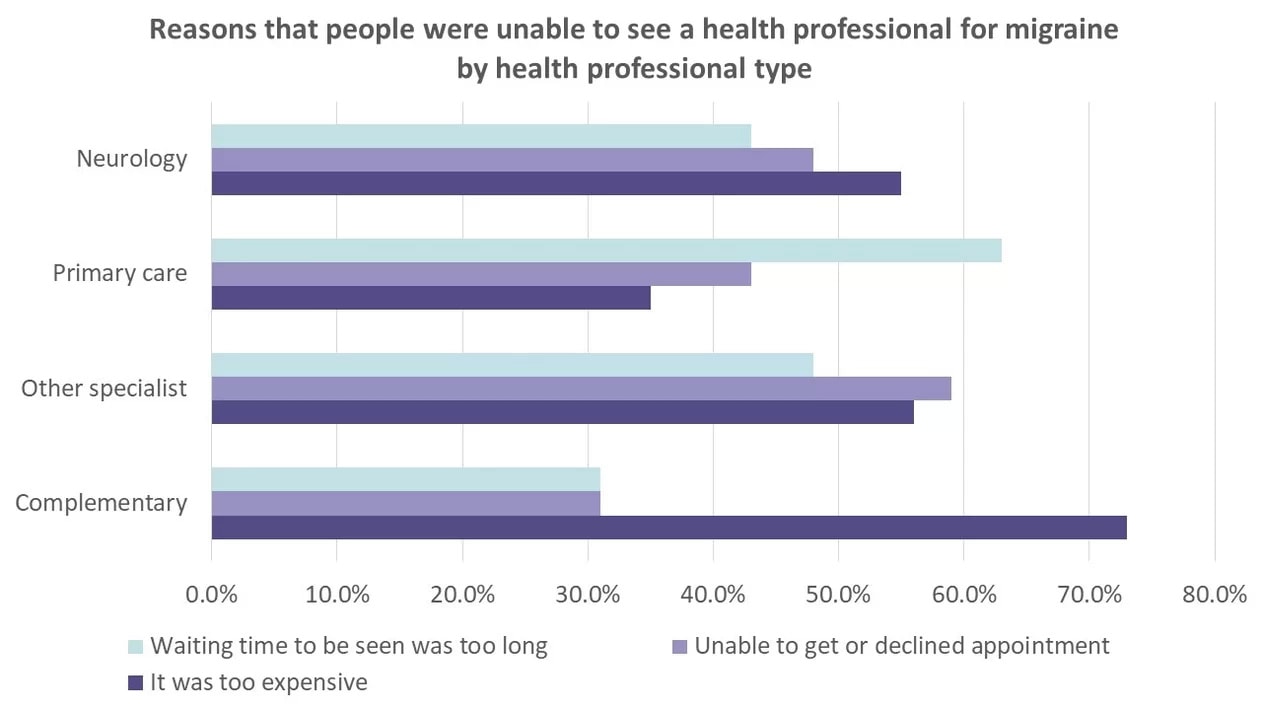
These were the top three reasons people were unable to be seen for migraine across the different types of health professionals (except for ED – there were not enough people who couldn’t see an ED clinician to look at this further. We hope this means that EDs are doing what they are there for – treating acute and emergency medical conditions, including people who are unable to see GPs and specialists.)
For neurologists, expense was the most commonly given reason; for primary care, the top reason was waiting time; for other specialists (e.g. pain specialist, endocrinologist), it was unable to get an appointment, although expense was a close second; for complementary care (e.g. osteopath, physiotherapist, massage therapist), expense was the standout reason.
We don’t want to pour burning coals upon the heads of health professionals who are already working extremely hard, often to the point of burnout. But this is another sign of a health system that is not meeting the needs of the people it is intended to serve.
It’s an election year, and we have the chance to put health firmly on the political agenda. Check out our election issues for 2023 – there are plenty of ideas in there which can be used to advocate for a better-functioning healthcare system, one that works for people with migraine as well as for any other health condition. You could use the information in this article, and other articles we’ve published using the Migraine in Aotearoa New Zealand Survey, to highlight the need for more timely, affordable and available health care for people with migraine.
If you’re finding it difficult to access health care, you could try reaching out for support and advice from our online migraine community – there is a heap of wisdom in our private Facebook support group. And we’re working on updating and expanding the information on our website. If there are things you want to know about that aren’t yet on the site, drop us an email at info@migrainefoundation.org.nz.