Even though they were developed to treat seizure disorders, anti-seizure medicines are commonly used for migraine prevention. However, they only work about half of the time and they are not easy to take, having multiple and often unpleasant side effects.
Anti-seizure medicines that can be recommended for migraine prevention include topiramate (Topamax), sodium valproate (Epilim), gabapentin (Neurontin) and lamotrigine (Lamictal).
From the Migraine in Aotearoa New Zealand Survey 2022, 30% (n=148) had previously used an anti-seizure medicine and 8% (n=40) were currently using an anti-seizure medicine for migraine prevention (from a sample of 489 people who answered these questions).
The most commonly used anti-seizure medicine was topiramate – 24 people were currently using it, and 128 had previously used it (Table 1). Most of these people had stopped because of side effects (n=85) or because it didn’t work (n=38). For the other anti-seizure medicines, the numbers of those who stopped because of side effects were fairly similar to those who stopped because they didn’t work.
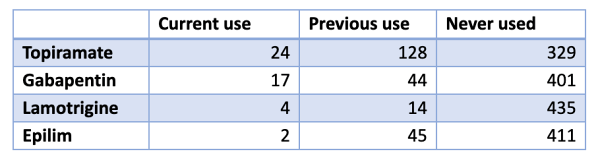
Table 1: Number of people using anti-seizure medication for migraine prevention, from Migraine in Aotearoa New Zealand Survey 2022
Another key risk to consider when you are a person of child-bearing potential who is taking anti-seizure medicines for any reason is that anti-seizure medicines can affect a developing fetus at any time during pregnancy. Congenital malformations (e.g. heart defects, cleft palate, spina bifida) are most likely to occur during the first three months of pregnancy, but neurodevelopmental effects can occur at any time, which may lead to cognitive, attention, learning and language difficulties. The fetus can be affected before a person even knows they are pregnant.
Fetal Anti-Convulsant Syndrome (FACS) occurs when an anti-seizure medicine taken during pregnancy crosses the placenta and into the developing fetus. The diagnosis of FACS can only be made by a specialist, and is only made when the childbearing person took an anti-seizure medicine during pregnancy, has a child with a combination of physical malformations, unusual physical features (often of the face) and neurodevelopmental difficulties with no other cause to explain these difficulties.
What to do about anti-seizure medicines for migraine prevention
If you are a person of child-bearing potential, try other migraine prevention options in preference to anti-seizure medicines, and avoid Epilim in particular. Other options include beta-blockers and some other anti-hypertensive medications, some anti-depressants and the new migraine-specific injectable calcitonin gene-related peptide blockers. Find out what migraine medications are available in New Zealand here.
If you take anti-seizure medicines for migraine prevention and could become pregnant, use two forms of contraception.
If you take anti-seizure medicines for migraine prevention and are planning to get pregnant, talk to your doctor/specialist about reducing or coming off the anti-seizure medicine.
If you take anti-seizure medicines for migraine prevention and you can’t get pregnant (e.g. you don’t have a uterus or you’re past menopause), then be aware of the risks for people of child-bearing potential who could be affected and talk to others who are taking these medications about these risks.
Written by Dr Fiona Imlach (MBChB, MPH, PhD), Migraine Foundation Aotearoa New Zealand Co-founder, and Denise Astil, Founder, Trustee and Executive Officer, Foetal Anti-Convulsant Syndrome NZ
Resources and further information


