Results from the Migraine in Aotearoa New Zealand Survey 2022
Hormones undoubtedly play a role in the manifestation of migraine. Before puberty, the prevalence of migraine is roughly equal between boys and girls but after puberty, migraine becomes more common in females.
Females experience changes in migraine related to female sex hormones, especially estrogen. Migraine attacks around the time of periods (menstrual migraine) are common and usually more prolonged and debilitating than other attacks. These attacks are caused by falling levels of estrogen just before the period and one way to prevent them is to take a combined oral contraceptive (estrogen and progesterone) continuously, without the seven-day hormone-free break. This isn’t recommended for people who have migraine with aura because of a small increased risk of stroke.¹ Another option is to take progesterone-only contraception, which is safe to use in all types of migraine.
Migraine often improves during pregnancy and after menopause (defined as when periods have totally ceased and the ovaries no longer produce eggs) but may worsen during perimenopause, those years of transition before menopause itself, when hormone levels (estrogen and progesterone) fluctuate and periods become irregular. Hormone replacement therapy (with low dose estrogen) can be used to even out these fluctuations and may help with migraine, or at least with other symptoms associated with perimenopause.²
The role of testosterone, the male sex hormone, in migraine is not well understood but may also play a role. For example, testosterone levels have been found to be lower in men with chronic migraine than in men without migraine.² ³
Finally, melatonin is a hormone that can be used for migraine prevention but is sometimes categorised as a supplement.⁴ Melatonin is involved in regulating sleep and circadian (day/night) cycles. At present, melatonin is only available in New Zealand through prescription from a doctor and isn’t sold online or over the counter as a supplement.
From the 2022 Migraine in Aotearoa New Zealand survey, 30% were currently using female hormones for migraine prevention (18% using progesterone only; 12% using estrogen with or without progesterone). A higher proportion had previously used these hormones but stopped, predominantly because of side effects. It’s worth noting that oral contraceptives can worsen headaches in some people, especially when taking the seven-day hormone-free break.
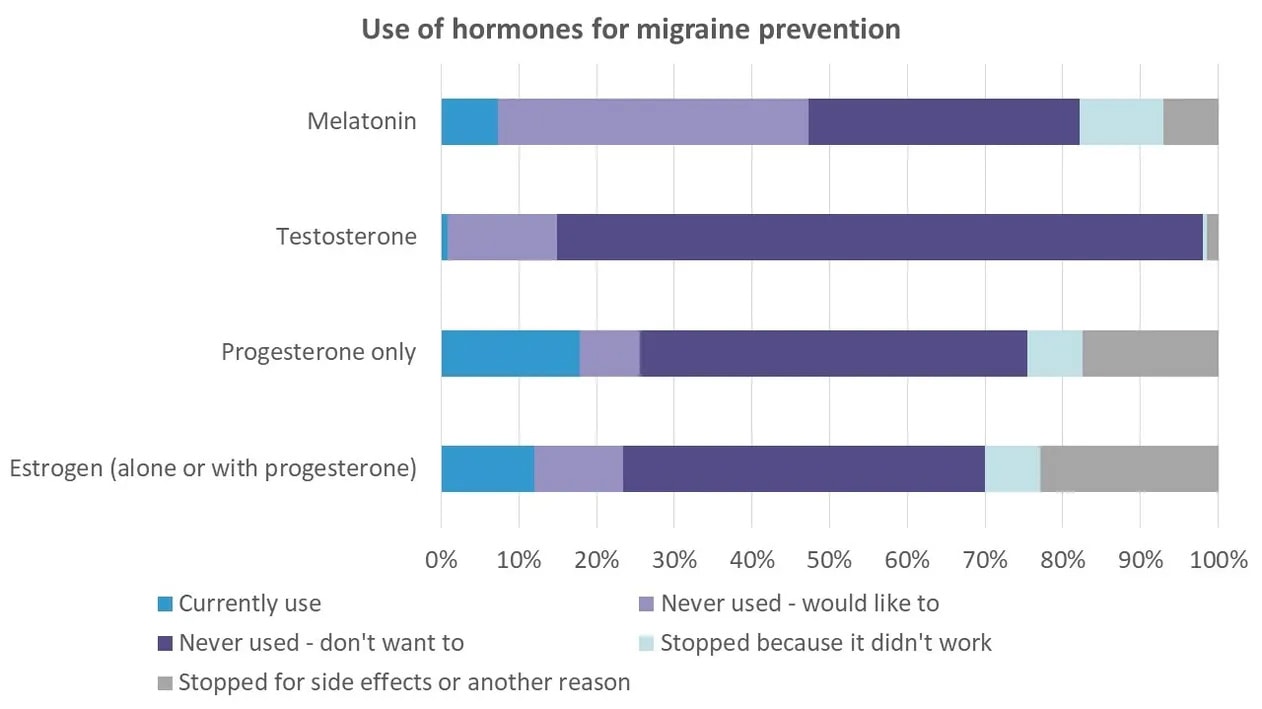
Few people (1%) were using testosterone and, appropriately, this wasn’t a treatment of interest for most (83% did not want to try this). More people (40%) were interested in trying melatonin, although only 7% were currently using it and 18% had previously tried it and stopped for various reasons.
The prevalence of menstrual migraine amongst women with migraine is estimated to be around 25% and older women with migraine may also take hormone replacement therapy, which is consistent with our finding that 30% of survey respondents were taking female hormones for migraine prevention. However, another 30% of respondents had stopped taking estrogen and 25% had stopped taking progesterone because of side effects, lack of effectiveness or another reason.
This raises the question of whether those people found an alternative treatment for hormonally-sensitive migraine attacks. There aren’t many options. For menstrual migraine, you can try taking non-steroidal anti-inflammatories before the period starts, or a long-acting triptan (naratriptan or frovatriptan). Unfortunately, we don’t have long-acting triptans in New Zealand, so this isn’t an option here. Naratriptan used to be available but is no longer, possibly because an application to Pharmac to fund naratriptan was declined in 2021 (after a huge delay – the application was made in 1997).
There’s a lot more we need to know about hormonally-sensitive migraine in New Zealand, especially menstrual migraine, including their impact on people and their treatment. But we already know that, as usual, New Zealand is behind on access to treatments used elsewhere.
References
- Grøtta Vetvik, K. & Anne MacGregor, E. Menstrual migraine: a distinct disorder needing greater recognition. www.thelancet.com/neurology 20, (2021).
- Ahmad, S. R. & Rosendale, N. Sex and Gender Considerations in Episodic Migraine. Curr Pain Headache Rep (2022) doi:10.1007/S11916-022-01052-8.
- Tsai, C. K., Tsai, C. L., Lin, G. Y., Yang, F. C. & Wang, S. J. Sex Differences in Chronic Migraine: Focusing on Clinical Features, Pathophysiology, and Treatments. Curr Pain Headache Rep 26, 347–355 (2022).
- Puliappadamb, H., Maiti, R., Mishra, A., Jena, M. & Mishra, B. Efficacy and Safety of Melatonin as Prophylaxis for Migraine in Adults: A Meta-analysis. J Oral Facial Pain Headache 36, 207–219 (2022).
Further reading
- Menstrual migraine treatment and prevention, American Migraine Foundation
- Menstrual migraine, The Migraine Trust