Results from the Migraine in Aotearoa New Zealand Survey 2022
In our Preventive Migraine Medications Use in Aotearoa New Zealand report, we reported on how many people from the Migraine in Aotearoa New Zealand Survey 2022 were taking medication for prevention (around half) and how many people with severely disabling and/or frequent migraine attacks were taking preventive medication.
Now we’ve analysed what types of medication people are or have previously taken for migraine prevention. There are many different medications that can be used, but all of these, excluding the new, migraine-specific medications targeting calcitonin gene-related peptide (CGRP), were initially developed and used to treat other conditions, such as hypertension, depression or epilepsy. It was only by chance, not design, that these medications were noted to have some efficacy in preventing migraine attacks.
In the survey, we specifically asked about medications included as options for migraine treatment in international guidelines (New Zealand doesn’t have its own migraine treatment guidelines at present). We asked whether people were currently taking any of these medications or whether they’d used them in the past for migraine but had stopped because of side effects because they didn’t work or for some other reason.
Use of the CGRP monoclonal antibodies (Emgality and Aimovig were available at the time of the survey) are discussed in a separate report, as are other injections, hormone treatments (including melatonin, estrogen and testosterone), supplements and non-medication approaches to migraine prevention.
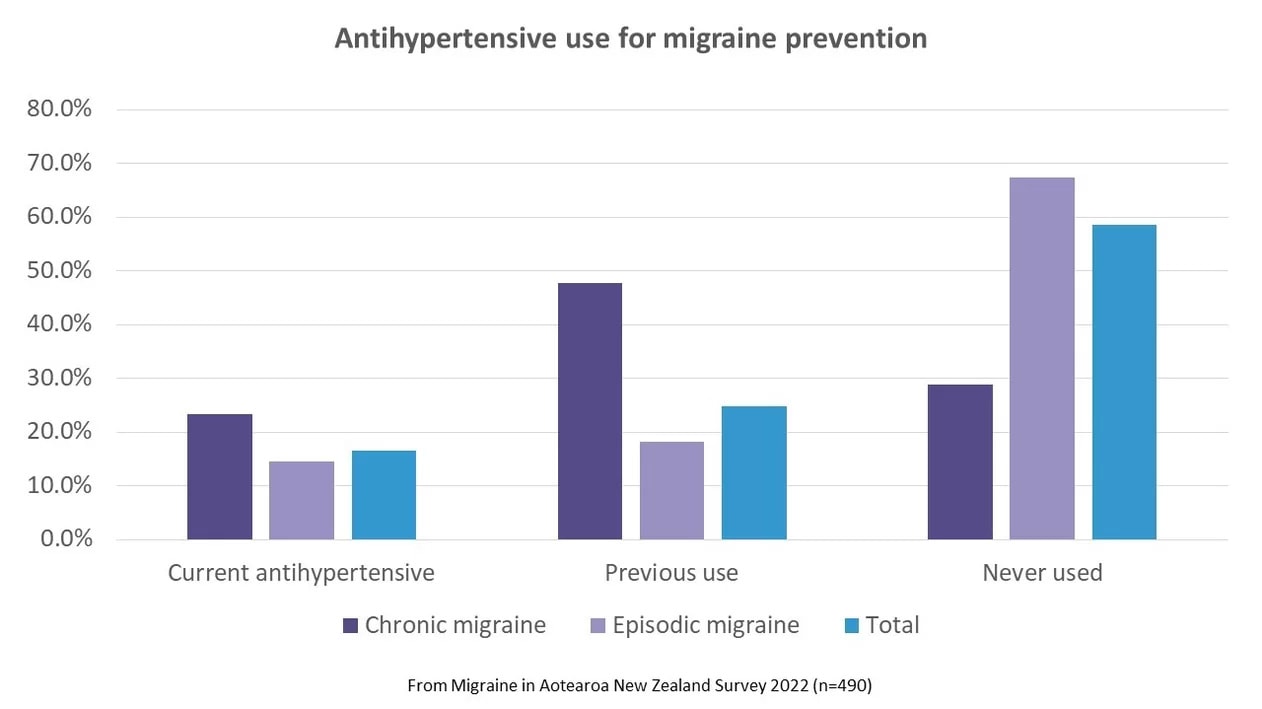
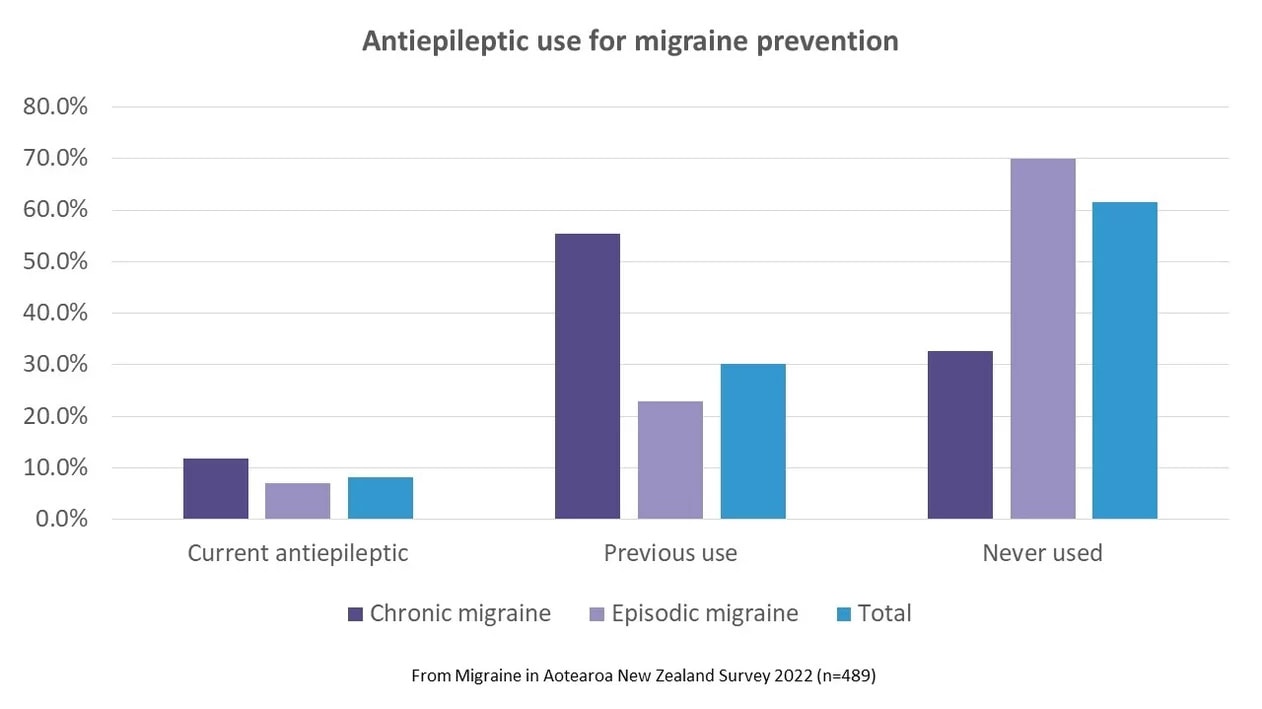
For all classes of preventive medication, people with chronic migraine (headache on 15 days or more per month) were more likely to be currently taking and to have previously taken that type of medication than those with episodic migraine (migraine on 14 days or less a month).
Antidepressants
Antidepressants were the most commonly used class of medication for migraine prevention, with 28% of the survey respondents currently taking an antidepressant for migraine, over a third (36%) having previously used one and the minority (37%) never having used one.
This relatively high use of antidepressants may be because anxiety and depression quite commonly co-exist with migraine and prescribers may choose to prescribe a medication that could treat both conditions – two birds with one stone. Also, migraine is most common in working-age people, particularly women, and prescribers may be more comfortable giving out antidepressants to this age group than antihypertensives, which are more often used in older people.
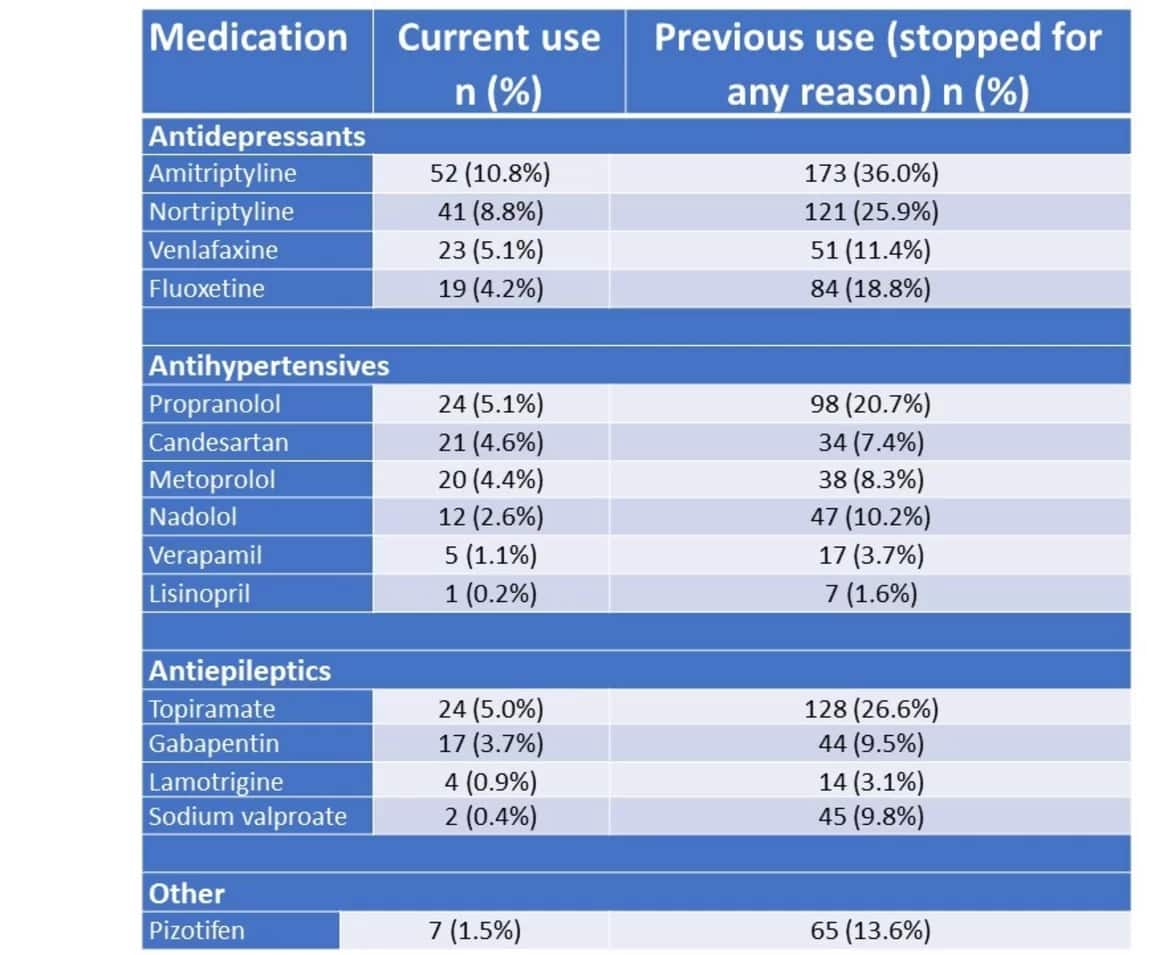
We specifically asked about amitriptyline, nortriptyline (both tricyclic antidepressants), venlafaxine and fluoxetine. Respondents also listed other antidepressants they’d used for migraine including citalopram, sertraline, paroxetine, mirtazapine and duloxetine.

Antihypertensives
The next most commonly used class of medications for migraine prevention was antihypertensives, including beta blockers, with 17% of survey respondents currently taking an antihypertensive medication for migraine and 25% having previously taken one.
We specifically asked about verapamil, candesartan, lisinopril, nadalol, metoprolol and propranolol. Respondents listed other antihypertensives used for migraine prevention, including cilazapril, quinapril, amlodipine and perindopril.
Antiepileptics
Only 8% of survey respondents were currently taking an antiepileptic for migraine prevention but 30% had previously taken one. We discuss the risks of taking antiepileptic medications for people with child-bearing potential in this article.
Rates of use of individual medications
The tricyclic antidepressants (amitriptyline and nortriptyline) were the medications that were most in current use, by 11% and 9% of respondents respectively (Table 1). They were also, along with topiramate, the medications that had been most often previously used, but stopped.
Topiramate was the most common antiepileptic in current use; candesartan, propranolol and metoprolol were most currently used amongst the antihypertensives.
From other research, many people are unable to tolerate the side effects of these medications or they discontinue using them because they’re only effective for about half of people who take them (‘effective’ in reducing headache days by around 50%). Our survey respondents stopped taking these medications for both of those reasons, in roughly equal measure, except for topiramate, where more than twice as many people said they stopped because of side effects rather than because it didn’t work. Side effects also appeared to be more problematic for venlafaxine, fluoxetine and amitriptyline.
The survey results show that the older migraine preventive medications are much more likely to have been used in the past, and stopped because they were ineffective or intolerable, than to be currently used.
This highlights the dire need for new and more effective medications to prevent migraine attacks, that have fewer side effects. The CGRP medications are the first of this type to be developed, with more being investigated and tested. In a recent systematic review, the CGRP medications outclassed the other drugs used for migraine prevention for both safety and efficacy.¹
If we can’t get the CGRP medications funded in New Zealand, we would have to seriously question how Pharmac applies its Factors for
Consideration (Need, Health Benefit, Suitability and Costs and Savings) to its decision-making.
References
- Lampl C, MaassenVanDenBrink A, Deligianni CI, Gil-Gouveia R, Jassal T, Sanchez-Del-Rio M, Reuter U, Uluduz D, Versijpt J, Zeraatkar D, Sacco S. The comparative effectiveness of migraine preventive drugs: a systematic review and network meta-analysis. J Headache Pain. 2023 May 19;24(1):56. doi: 10.1186/s10194-023-01594-1


