Results from the Migraine in Aotearoa New Zealand Survey 2022
Migraine isn’t fatal but it does cause disability. There’s a measure of disability called Years Lived with Disability (YLD), which measures the burden of living with a non-fatal disease at a population level, allowing different diseases with different impacts to be compared with each other.
For migraine, it combines the prevalence of migraine disease, the average time spent in a migraine attack per year (estimated from population-based studies to be 8.5% of a year) and a disability weight.¹ The disability weight is taken from multiple surveys of people who rank different health states to come up with a number that reflects the severity of the disability. From 2019 burden of disease models, the disability weight for migraine was 0.441, which means that during a migraine attack, a person experiences a health loss of 44.1% compared with someone in full health.²
Some conditions with similar disability weights include severe dementia (0.449), most severe back pain (0.372), severe cocaine dependence (0.479) and moderate depressive episode (0.396).²
Using the YLD measure, it’s estimated that migraine disease is the second highest cause of disability globally and ranks as the fourth highest cause in Aotearoa New Zealand, neck-and-neck with depression and not far behind anxiety disorders. But we can also measure disability from migraine at an individual level. One commonly used method is the Migraine Disability Assessment Scale (MIDAS).³ ⁴ This uses a set of questions tested and used in migraine drug trials, that measure the impact of migraine attacks on daily life. The questions are:
1. On how many days in the last 3 months did you miss work or school because of your headaches?
2. How many days in the last 3 months was your productivity at work or school reduced by half or more because of your headaches? (Excluding days counted in question 1)
3. On how many days in the last 3 months did you not do household work (such as housework, home repairs and maintenance, shopping, caring for children and relatives) because of your headaches?
4. How many days in the last 3 months was your productivity in household work reduced by half of more because of your headaches? (Excluding days counted in question 3)
5. On how many days in the last 3 months did you miss family, social or leisure activities because of your headaches?
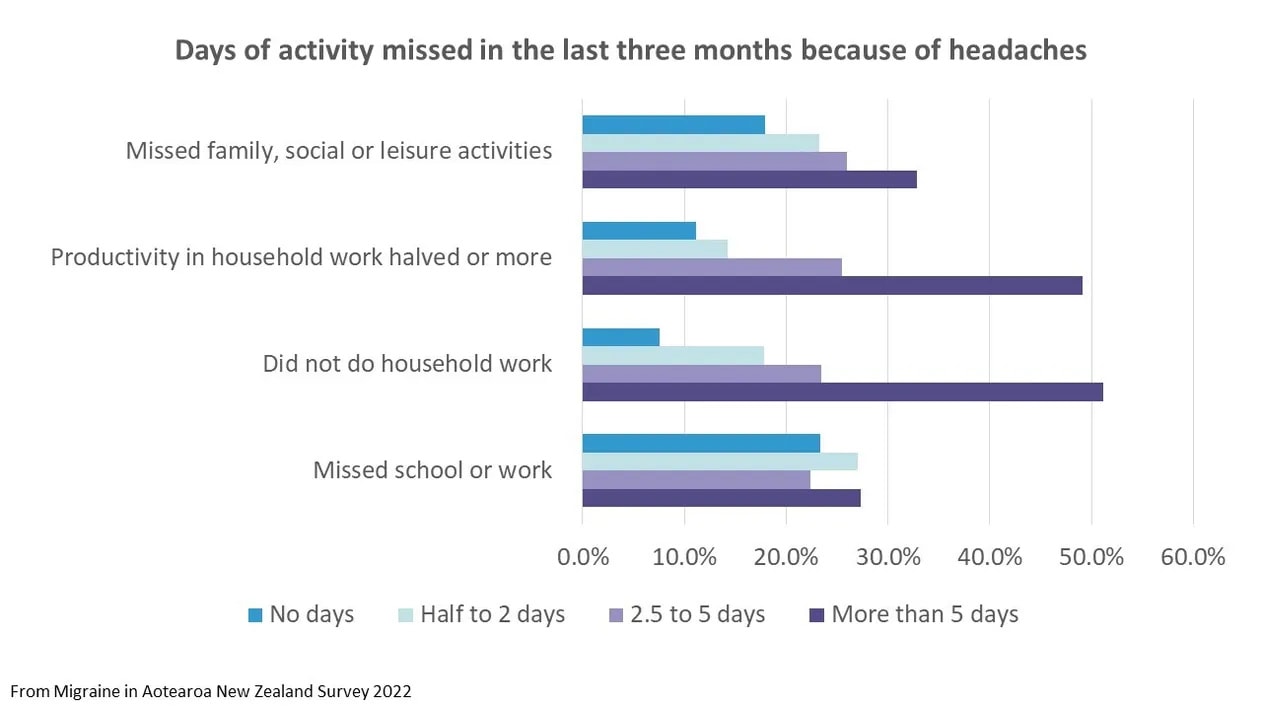
We asked four of these questions in the Migraine in Aotearoa New Zealand Survey 2022 and found a huge impact on activities from migraine:
- Half of respondents hadn’t been able to do household work on more than five days in the last three months.
- Nearly a third had missed family, social or leisure activities on more than five days.
- Over a quarter had missed school or work on more than five days.
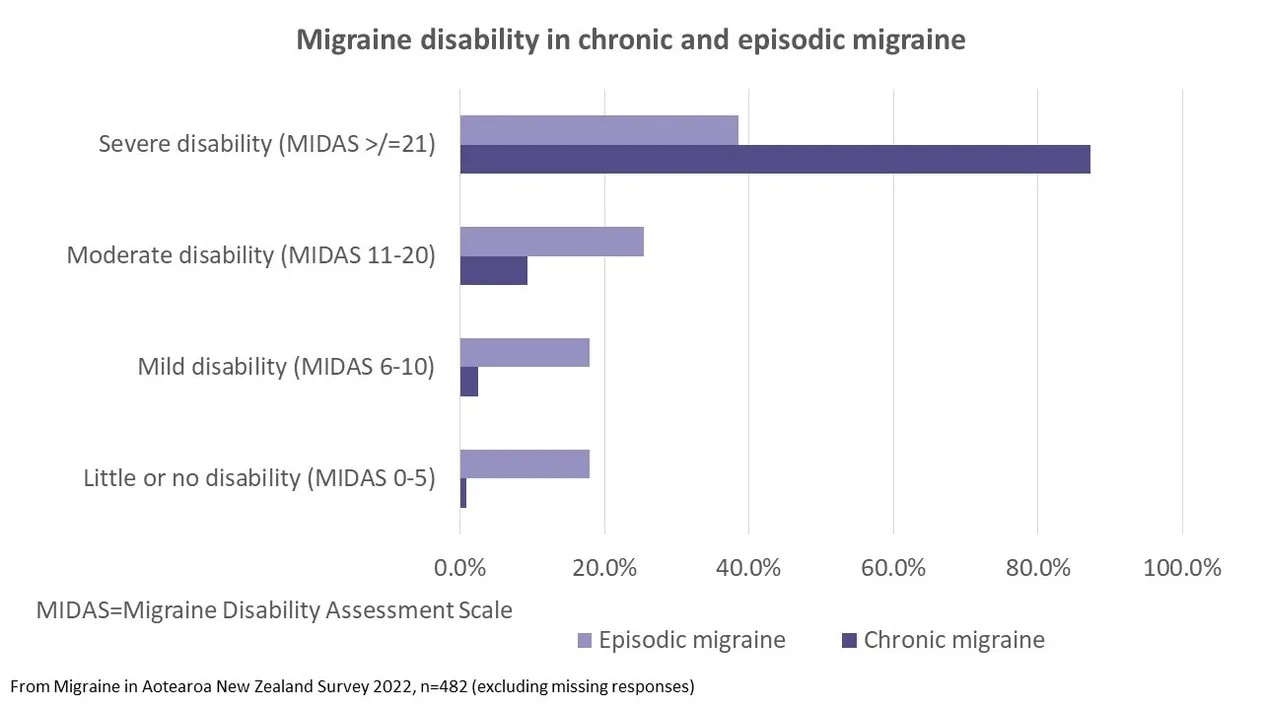
The MIDAS can be used to categorise people into levels of disability, depending on the number of days that headaches impact on activities. A score of 21 or more indicates severe disability – at least 21 days in the last three months that were negatively affected by headaches. Given we didn’t ask one of the five MIDAS questions, the scores from our survey will under-estimate disability compared to other studies, but we still see a high proportion of people with severe disability – nearly half (49%) overall and 87% of people with chronic migraine had severe disability.
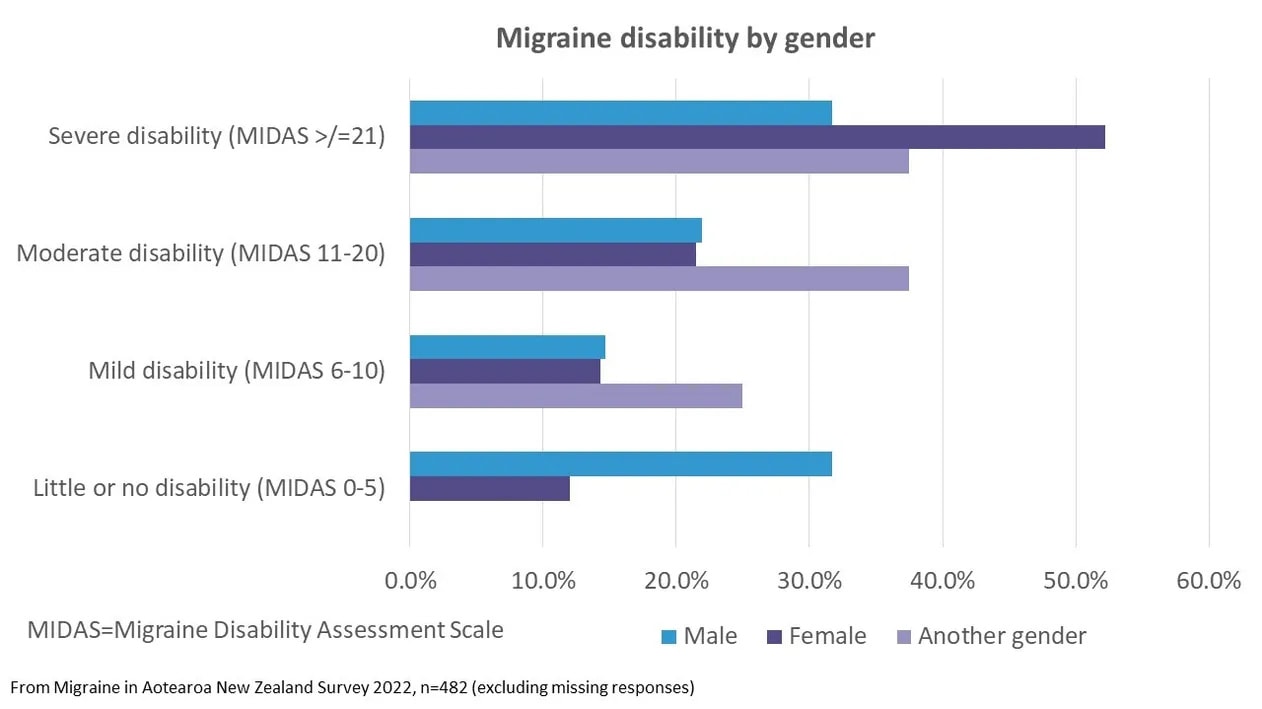
There was also a difference by gender, with a higher proportion of females (52%) with severe disability compared with males (32%). There were only 8 people of another gender in the survey, so the proportions for these people will be imprecise but are trending towards a higher level of disability. Other studies have reported a higher disability from migraine and more frequent headache days in women.⁵
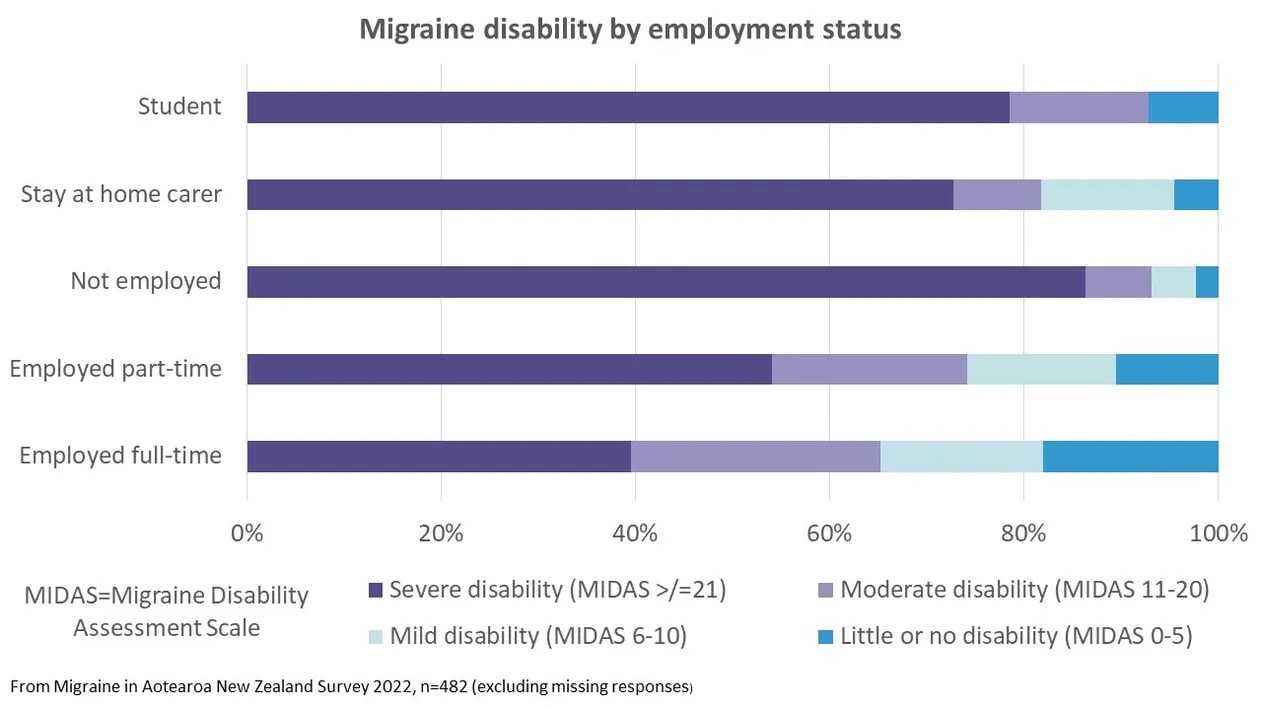
Not surprisingly, migraine disability was related to employment status. People in full-time employment had the lowest levels of severe disability (40%) and those who were unemployed had the highest (86%). Reducing the impact of migraine could make it possible for some people to find employment and also improve the productivity and enjoyment of work in those who are employed but have high levels of disability.
The disability from migraine is often under-rated but these results show the marked impact of migraine on the lives of people in New Zealand. Migraine may be a non-fatal disease, but with disability levels this high, some people might wish it were.
A snapshot of what some survey respondents said about migraine disability:
“At times I have felt defeated by the constant pain and this has impacted my mental health. I can’t imagine the life I might have had without migraine. It is like living with an invisible disability.”
55–64 year old NZ European female
“With a working partner I am ineligible for [disability] support but migraine are so debilitating that I feel incapable of working.”
45–54 year old NZ European female
“Recently I broke my elbow. That was very painful. The migraine I experience are significantly more painful than breaking my elbow. Migraines are also significantly more disruptive to my life than not being able to use one of my arms. If I could cut off one of my arms and never experience migraine again I would do it in a heartbeat”.
35-44 year old NZ European male
Anyone who says that migraine is ‘just a headache’ and ‘just take a pill’ needs to start paying attention to the reality of what living with migraine can be like. Or they may like to visit our Voices of Migraine page to better understand the challenges of living with migraine.
References
1. Stovner, L. J. et al. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 17, 954–976 (2018).
2. Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Disability Weights. (2020).
3. Stewart, W. F., Lipton, R. B. & Kolodner, K. Migraine disability assessment (MIDAS) score: relation to headache frequency, pain intensity, and headache symptoms. Headache 43, 258–265 (2003).
4. Stewart, W. F., Lipton, R. B., Simon, D., Liberman, J. & Von Korff, M. Validity of an illness severity measure for headache in a population sample of migraine sufferers. Pain 79, 291–301 (1999).
5. Ahmad, S. R. & Rosendale, N. Sex and Gender Considerations in Episodic Migraine. Curr Pain Headache Rep (2022) doi:10.1007/S11916-022-01052-8.


