Current issues & challenges

In recent years, treatment and knowledge about migraine have improved globally
The number and variety of treatments for migraine have expanded greatly in past years. People with migraine no longer have to take medications that were developed for other diseases; there are now treatments specifically targeted at migraine.
These include medications to treat migraine attacks when they occur (acute treatments), medications to prevent attacks from happening (preventive treatments) and devices that may treat or prevent attacks.
However, people with migraine in Aotearoa are disadvantaged by limited medication and treatment options, far behind what is available in Australia and the UK. There is also limited New Zealand-specific migraine information, a dire lack of research, limited access to migraine-specific care, and a general under-appreciation of the true impact of migraine disease, with high levels of migraine stigma.
Migraine landscape in Aotearoa
Many people don’t understand what migraine disease is, how it can be treated and how it affects people. For example, many people are unaware that migraine is a hereditary condition that often runs through families.
Common myths about migraine disease include that migraine is a women’s problem, eliminating certain foods from your diet will stop migraine attacks, or headache medication will cure migraine. However, many men also get migraine, diet is complicated (for example, craving chocolate and cheese are often part of the early stage of a migraine attack, rather than causing it; caffeine can help treat a migraine attack, but caffeine withdrawal can trigger one) and there is no cure for migraine, despite what some people claim – although it can be managed successfully.
The most common myth, that migraine is ‘just a headache’, can lead to misunderstandings about the severity and impact of migraine disease. The effects of a migraine attack can last for hours to days, beyond the headache stage, and other symptoms of a migraine attack can be as debilitating as the headache, including nausea and vomiting, visual disturbances, light and sound sensitivity, brain fog, speech difficulties, fatigue and mood changes.
It’s not only the general public who don’t have a good understanding of migraine disease. Health professionals may not know how to distinguish migraine from other headache conditions, or be aware of the best management options. Dr Katy Munro, a headache specialist GP in the UK says, “Many doctors lack training in migraine diagnosis and treatment” and Dr Tissa Wijeratne, a neurologist in Australia, says that, “migraine is … the least respected and worst managed medical disorder worldwide”.
Without a broad and widespread understanding about migraine disease among society, health professionals, employers, educators and others, people with migraine in New Zealand can struggle to get diagnosed, and get the treatment and support they need to manage migraine in the best possible way.
People with migraine in Aotearoa New Zealand often face difficulties in accessing neurologists or other headache specialists, especially if they can’t afford private health care. There is a shortage of health professionals with specialised knowledge about migraine. For example, the Australia and New Zealand Headache Society (ANZHS) keeps a directory of clinicians with an interest in headache. As of 2022, there were only four in New Zealand. A New Zealand online health service directory also lists only three neurologists (some different ones than from the ANZHS directory) with a specified interest in migraine.
We know there are many more neurologists and specialists who are interested in migraine disease, but it can be difficult to find them.
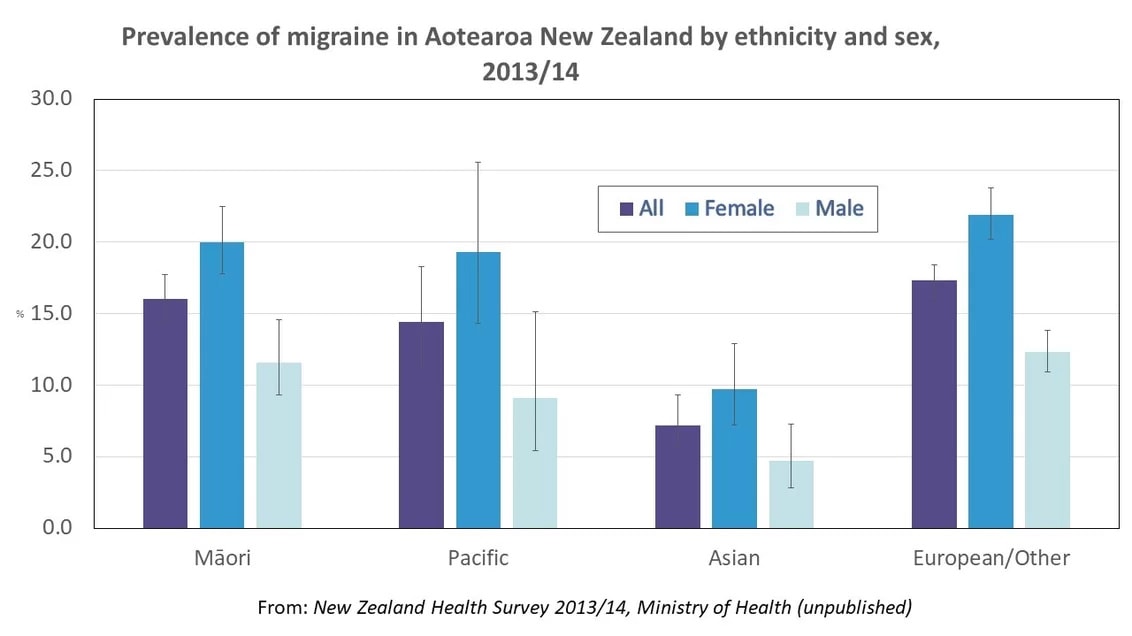
The proportion of a population who has a specific disease in a given time period is known as ‘prevalence’. The most recent estimates of the prevalence of migraine in New Zealand come from the 2013/14 New Zealand Health Survey (NZHS) and the Global Burden of Disease 2023 study.
The NZHS found an overall prevalence of 15.7%, which varied by age and gender. This survey asked whether participants had been told they had migraine by a doctor and did not ask specific questions about migraine symptoms, meaning people with undiagnosed migraine may have been missed. We also cannot identify the proportion of people who are currently experiencing migraine attacks or those who are severely impacted by migraine attacks.
The Global Burden of Disease 2023 study estimated that around 15% of people in New Zealand had migraine (12% in males and 18% in women), which is similar to global estimates. This was a measure of annual prevalence (how many people experienced the disease in one year). This equated to over 730,000 people in 2023 in New Zealand and over a billion people worldwide.
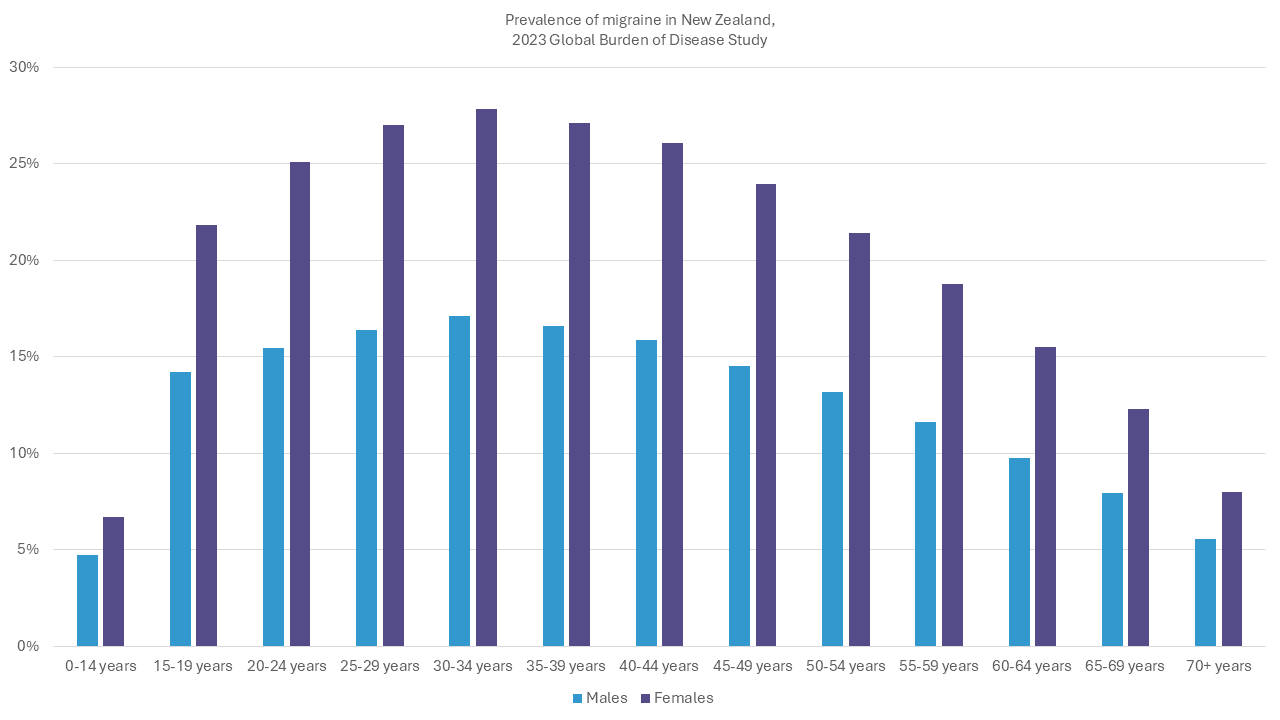
Based on Global Burden of Disease 2023 data, available at https://vizhub.healthdata.org/gbd-results/, accessed June 2024
In New Zealand, migraine disease is more common than many other conditions that cause pain or affect the brain and is more prevalent than diabetes, epilepsy and stroke combined.
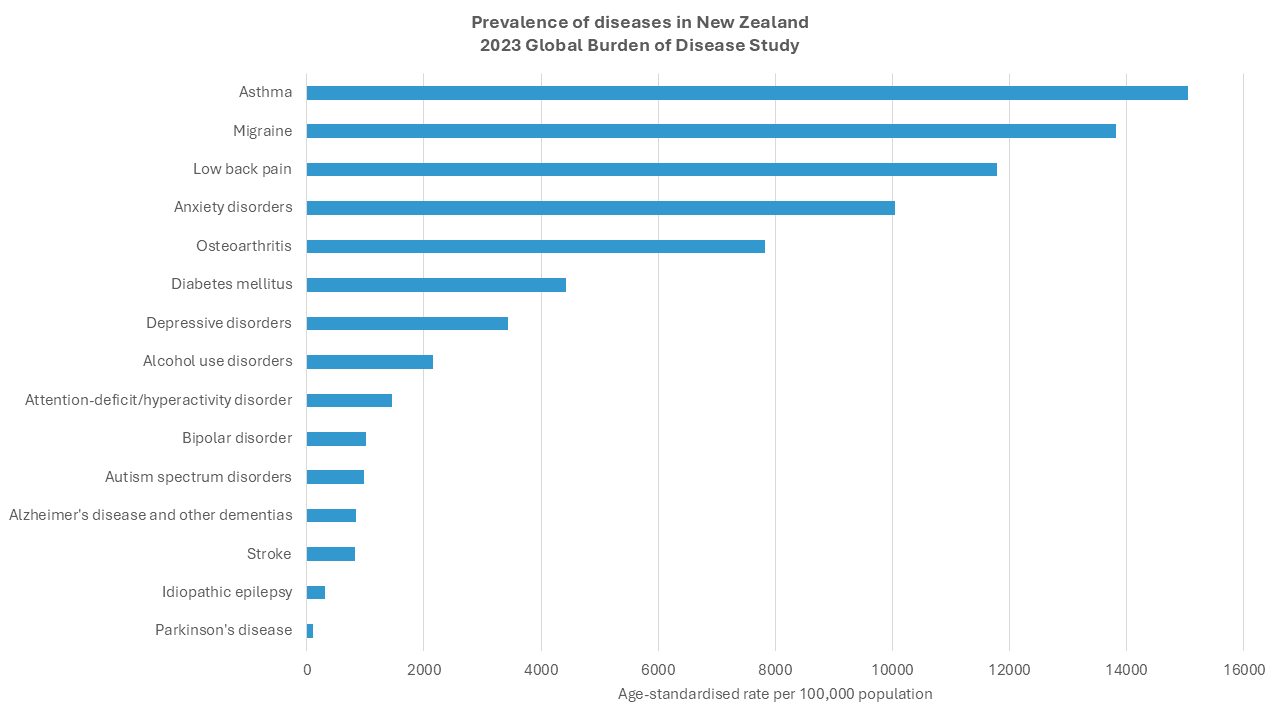
Based on Global Burden of Disease 2023 data, available at https://vizhub.healthdata.org/gbd-results/, accessed October 2025
Our best estimate of the prevalence of migraine disease in Māori or Pacific people in New Zealand comes from the 2013/14 New Zealand Health Survey (NZHS). This found a similar overall prevalence of migraine in Māori (16%), non-Māori (17%) and Pacific people (14%). The lower prevalence in Pacific people was not statistically significant but other research has found that Pacific people are less likely to be diagnosed with migraine, despite having migraine symptoms.
Research from the United States has found that indigenous people have the highest prevalence of migraine of all ethnic groups, and migraine is more common in people who live in poverty.
The burden of migraine disease in these ethnic groups, or any other communities in New Zealand, is unknown.
Given the well-documented inequalities in health outcomes for Māori (and Pacific people) in New Zealand, it’s probable that migraine is not as well recognised and managed in Māori and Pacific people and that the impact of migraine is greater. All New Zealand-specific research and information about migraine must consider and address these inequalities.
Despite a growing awareness of the impact of migraine globally, and the development of migraine-specific treatments, we know very little about the burden of migraine disease in New Zealand and very little research has been done on migraine in New Zealand.
The Health Research Council (HRC) is the primary source of Government funding for general health research and spends millions of dollars each year. The HRC has an online library of research projects that it has funded over the past ten years. A search in November 2021 found just one project with relevance to migraine – a study worth $500,000 looking for a new target to treat neurological pain. This study was classified as a ‘rheumatology/arthritis’ study because its main focus was on low back pain.
From the charitable sector, the Neurological Foundation is New Zealand’s leading charity that supports neurological research. The Neurological Foundation’s 50th anniversary publication in 2021 reported having allocated only $147,000 to migraine, headache and tinnitus research (combined) in 50 years, from a total funding pool of nearly $52 million. This is despite migraine causing the second highest burden of disability in the world, in global rankings of disease. The only other neurological condition with a similar burden of disability is depression, which commonly co-exists with migraine.
However, the Neurological Foundation did fund a migraine-specific project at the end of 2021 for just over $190,000. This project is looking at calcitonin gene-related peptide (CGRP) receptors in the brain to try and better understand why the new CGRP migraine medications don’t work for everyone.
In 2023, Professor Debbie Hay, Department of Pharmacology and Toxicology, University of Otago, was awarded $941,000 from the Marsden Fund for research into CGRP receptors and their relationship to migraine disease.
We have also undertaken our own research, beginning with our 2022 Migraine in Aotearoa New Zealand survey.
We need research like this, and so much more.
Access to medications
How medications are approved in New Zealand
For medicines and devices to be available in New Zealand, they must be approved by Medsafe, the agency responsible for assessing the safety and efficacy of all medical products.
Once approved by Medsafe, a product may be considered for funding by Pharmac, the agency responsible for deciding which products are subsidised for use in the community and in hospitals.
Products that have been approved by Medsafe but are not funded by Pharmac may be purchased at full price, if these are distributed and made available for sale by the pharmaceutical company that makes them.
Access to triptans
Triptans are abortive medications that can be taken by mouth, nasal spray or injection to treat a migraine attack. They were the first abortive medications developed specifically for migraine.
There are currently seven triptans available globally to treat a migraine attack, including five short-acting, one medium-acting and one long-acting. This gives people a range of options to help abort a migraine attack, as different triptans may be more or less effective for an individual, or have different side effects.
Only two triptans are funded and available in New Zealand. Both are short-acting. If neither of these medications are effective, there are no other migraine-specific abortive medications available for people in New Zealand to try.
In March 2022, after languishing on Pharmac’s application list for nearly 10 years, additional triptans including frovatriptan, naratriptan and zolmitriptan were declined for Pharmac funding.
Access and funding for Calcitonin Gene-Related Peptide (CGRP) monoclonal antibody medications
Calcitonin gene-related peptide (CGRP) monoclonal antibodies are the first medications developed specifically to prevent migraine. They have been found to be safe and effective, with fewer side effects than many other preventive migraine medications. They are taken by injection.
The CGRP monoclonal antibodies block a small protein called CGRP that helps to transmit pain signals in the brain, ramp up inflammation and dilate blood vessels. The CGRP monoclonal antibodies bind to CGRP or to its receptor sites found in some parts of the nervous system, effectively turning off its ability to stimulate the cascade of events that lead to a migraine attack.
Since May 2018, the US Food and Drug Administration (FDA) has approved three injectable CGRP medications and one CGRP infusion:
- Aimovig (erenumab)
- Emgality (galcanezumab)
- Ajovy (fremanezumab)
- Vyepti (eptinezumab)
Aimovig, Emgality and Ajovy are given once a month by self-injection. Ajovy also has the option to use quarterly, with three injections four times a year. Vyepti is a one-hour intravenous infusion every three months.
In Australia, Emgality, Vyepti and Ajovy have been approved on the Pharmaceutical Benefits Scheme (PBS, similar to Pharmac in New Zealand), which means people in Australia now have funded access to all three. Aimovig is available privately. In the UK, Aimovig, Emgality, Vyepti and Ajovy are all available through the National Health Service for people with migraine who have not had success with three other preventive treatments.
Aimovig
Medsafe has approved Aimovig and it is available as a 70mg and 140mg dose. It’s available on prescription, but it’s not funded and a 70mg injection costs $678 and 140mg costs $1,356.
Aimovig is listed on Pharmac’s Options for Investment list.
Emgality
Medsafe has approved Emgality and it is available as a 120mg dose (cost may vary, from $325). Two injections (240mg) are given initially, then one every 4 weeks. Your GP can prescribe Emgality for you – it doesn’t require a neurologist prescription. Your GP may want to find out more information about it if they’re not familiar with prescribing it, because it only became available in New Zealand in September 2022.
Emgality should be available through any chemist in New Zealand. The wholesaler is CDC Pharmaceuticals, but even pharmacies that don’t usually purchase medicine from CDC can still get Emgality through them. Prices may vary, depending on the pharmacy.
Please visit our Emgality Advocacy Toolkit to learn more about advocating for funding in New Zealand, and our Emgality Frequently Asked Questions.
Emgality is listed on Pharmac’s Options for Investment list.
Ajovy
Ajovy has been approved by Medsafe and became available in New Zealand in January 2026.
Ajovy is administered by subcutaneous injection (an injection just under the skin). However Ajovy is the only injectable with two dosing options – either one injection (225mg) once a month, or three injections (675mg) every three months. Ajovy doesn’t require a loading dose.
Ajovy is available via prescription. General Practitioners and Nurse Practitioners can prescribe Ajovy, you don’t need a prescription from a neurologist. The Medsafe Data Sheet states that Ajovy should be initiated by a physician experienced in the diagnosis and treatment of migraine. Ajovy is available from any pharmacy throughout New Zealand as both CDC Pharmaceuticals and ProPharma are suppliers.
Ajovy costs around $300–$330 per 225mg/1.5ml injection.
Ajovy is listed on Pharmac’s Options for Investment list.
Vyepti
Vyepti has not been approved by Medsafe and according to Lundbeck there are no plans to make Vyepti available in NZ.
Access and funding for gepants and ditans
Gepants and ditans are new oral migraine medications that have been specifically developed to treat migraine. Ditans are similar to triptans and are used to treat migraine attacks but unlike triptans, ditans do not constrict blood vessels and may be used by people with heart or blood vessel diseases.
Gepants are a type of calcitonin gene-related peptide (CGRP) inhibitor that can be used to treat migraine attacks. Gepants are an option for people who cannot take or tolerate triptans or for whom triptans don’t work. Rimegepant and ubrogepant come in tablet form and zavegepant is a nasal spray.
Some gepants (rimegepant and atogepant) can also be used as a preventive migraine medication. This is the first type of medication that can be used to both treat and prevent migraine attacks. Another advantage of gepants is that they do not appear to cause medication overuse headache, unlike other acute migraine treatments.
Currently, four gepants are on the market:
- Ubrogepant (Ubrelvy)
- Rimegepant (Nurtec ODT)
- Atogepant (Aquipta)
- Zavegepant (Zavzpret)
Lasmiditan, the first ditan to be approved for use in 2019, was discontinued in November 2025. No other ditans are available for use.
As of 2026, four gepants are available in the USA. Atogepant and rimegepant are funded in the UK; rimegepant is available in Australia but is not funded. In November 2025, Lasmiditan was discontinued.
In October 2024 the first gepant atogepant (Aquipta) became available in New Zealand. Find out more here. No other gepants are available.
Funding for Botox injections to prevent migraine
Botox (onabotulinumtoxinA) injections have been found to reduce headache frequency and severity in people with chronic migraine (at least 15 headache days a month).
In 2010, the US Food and Drug Administration (FDA, similar to Medsafe in New Zealand) approved the use of Botox in people with chronic migraine.
Botox is funded for the prevention of headaches in people with chronic migraine in many other countries including Australia, the UK and parts of Canada.
Pharmac agreed to fund Botox for use in public hospitals in 2017 for a range of conditions, not just chronic migraine. However, most public hospitals have chosen not to fund Botox for people with chronic migraine, or have restricted access, so that most people in New Zealand cannot access funded Botox.
Self-funded Botox costs approximately $1,200 per session, and requires one session every 12 weeks.
Access to neuromodulator devices
Neuromodulation uses non-invasive electrical currents or magnetic pulses to change the activity of the nerve pathways in the brain. Neuromodulation can help to turn down brain activity involved in migraine pain and decrease the frequency of migraine attacks.
Different types of neuromodulator devices work in various ways, including stimulation of specific nerves (e.g. the trigeminal nerve in the face, the vagus nerve in the neck, or the occipital nerve in the back of the head) or more general stimulation of the brain. Most neuromodulator devices can be used as both acute and preventive treatment.
Overseas there are a range of neuromodulator devices available, such as CEFALY, Relivion, GammaCore Sapphire and Nerivio, which can be used at home to help prevent a migraine attack or during a migraine. More invasive nerve stimulation options are also available.
Mynd Migraine Relief, a transcutaneous electrical nerve stimulator (TENS) neuromodulator, was available through a New Zealand supplier until December 2021. Since then, people in New Zealand have had difficulty accessing it without a New Zealand contact.
Qalm, by PainGone, is a similar TENS device that was available in New Zealand until 2024 when distribution in New Zealand was discontinued.