Results from the Migraine in Aotearoa New Zealand Survey 2022
Most people who have frequent migraine attacks have been warned of the risks of “overusing” acute medication. We’re told that taking too many painkillers or triptans can end up causing a headache, instead of relieving it, resulting in a daily or near-daily “medication overuse headache” or “medication adaptation headache”.
This is also sometimes known as “rebound headache” but we prefer not to use this terminology because rebound headache is also used to refer to a migraine attack that recurs after an initially successful treatment. In this sense, rebound headache is very common, because migraine attacks can last for 72 hours (or even longer) and treatments for migraine attacks can wear off after a few hours, so it’s not unusual to have to take several doses of acute medication to completely treat a single migraine attack.
This is a completely different phenomenon from medication adaptation headache, which, according to accepted diagnostic criteria, can only be present with overuse of acute medications for at least three months.
The International Headache Society (IHS) has indicated people are at risk of medication adaptation headaches if they have headaches for 15 days or more a month (chronic migraine) and have used (for at least three months):
- simple analgesics on ≥ 15 days a month (including paracetamol, non-steroidal anti-inflammatories, combination analgesics and caffeine)
- opioids or triptans on ≥ 10 days a month.
Not all health professionals believe medication adaptation headache is a serious concern and others have raised questions about the ‘days per month’ thresholds, noting that some patients can take medication on more than 10 or 15 days a month and never develop medication adaptation headache; alternatively, some patients may develop medication adaptation headache when taking medications on fewer days.
Regardless of these debates, people with chronic migraine are often cautious about taking too many acute medications, not only because of the risk of medication adaptation headache but because of potential side effects of the medications themselves or just not wanting to be reliant on drugs to get through the day.
We had no information about the use of acute medications among people with migraine in New Zealand, until the Migraine in Aotearoa New Zealand Survey 2022. From this survey, 520 people answered all the questions about acute medications.
We asked about medication use in the last month and since medication adaptation headaches can’t be diagnosed without three months of medication overuse, our results only give a rough indication of how many people may be at risk of medication adaptation headaches and will likely overestimate the true risk. Still, it’s a level of insight we haven’t had before.
We calculated people at risk of medication adaptation headaches by identifying anyone who had reported using one or more of:
- paracetamol OR non-steroidal anti-inflammatories (NSAIDs e.g. aspirin, ibuprofen, diclofenac, naproxen, celecoxib, meloxicam) on at least 15 days in the last month for a migraine attack; OR
- triptans (e.g. rizatriptan or sumatriptan) OR opioids (e.g. codeine, tramadol, oxycodone) on at least 10 days in the last month for a migraine attack.
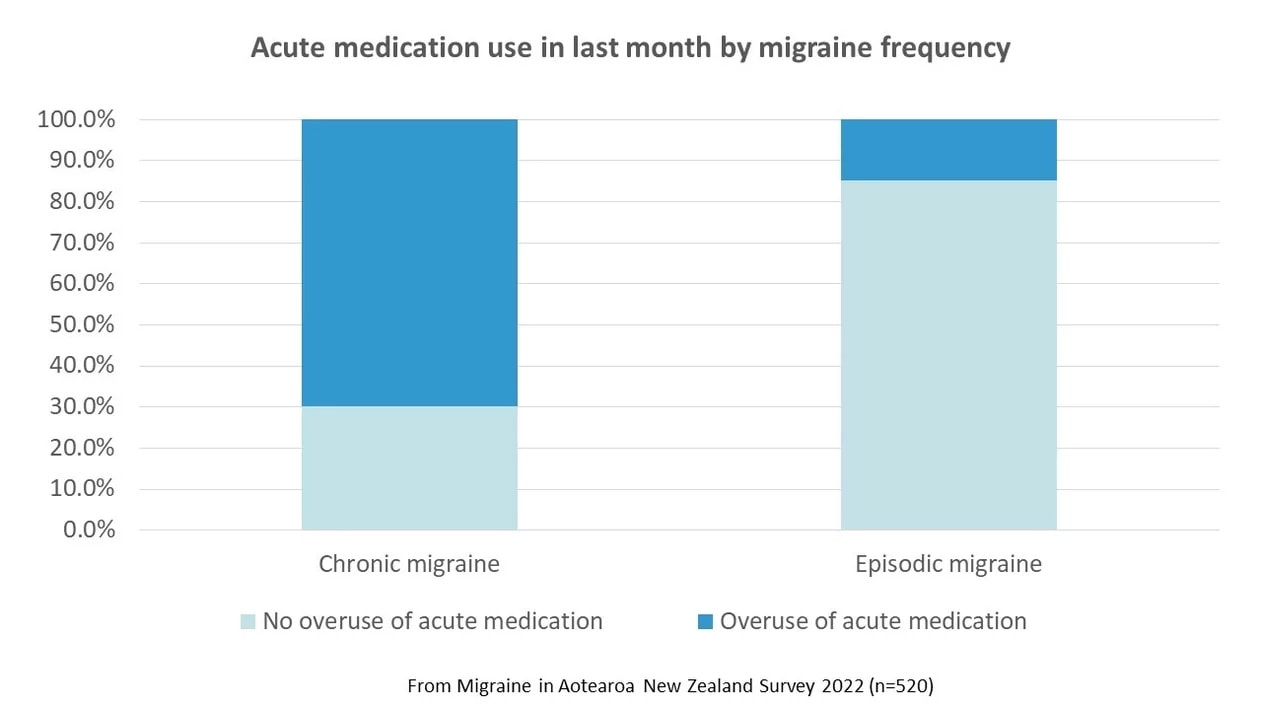
From this calculation, 27% of survey respondents could be at risk of medication adaptation headaches. Unsurprisingly, the risk was higher in people with chronic migraine than episodic migraine (and according to the IHS definition, medication adaptation headache only occurs in people with chronic migraine). 70% of people with chronic migraine had acute medication overuse in the last month, compared with only 15% of people with episodic migraine.
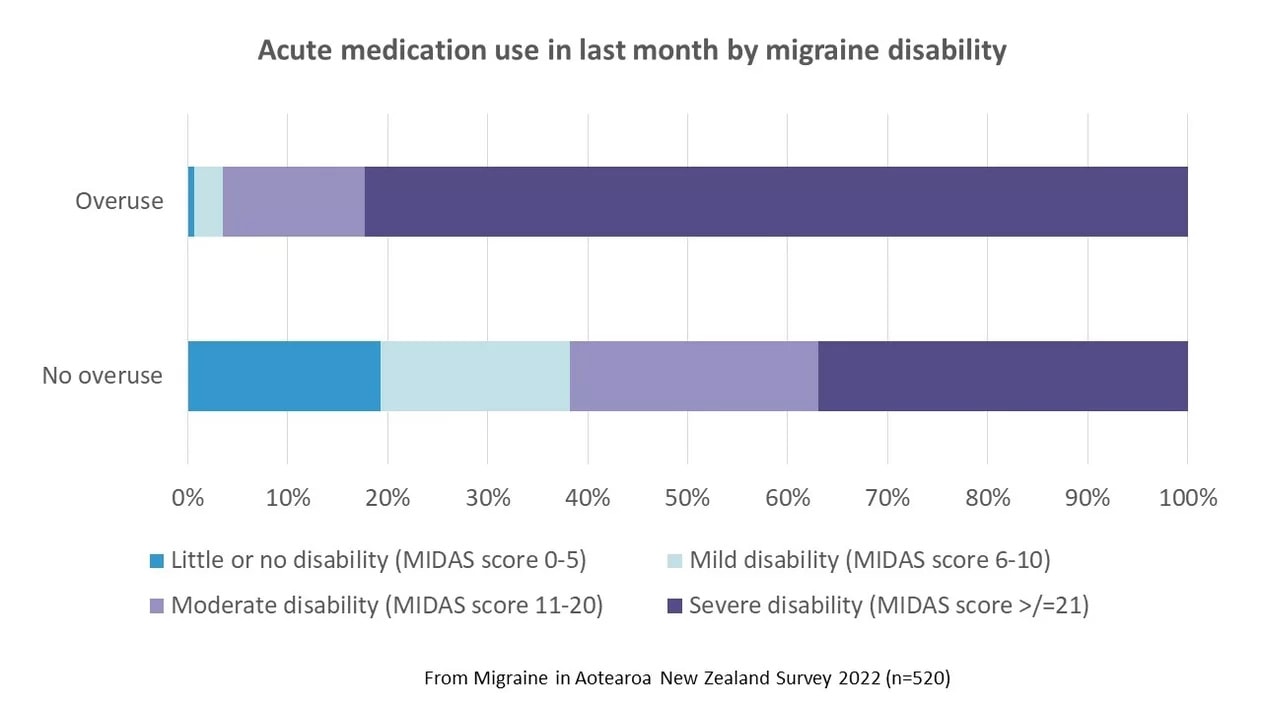
Chronic migraine is associated with more migraine-related disability and so is the risk of acute medication use. From the survey, the higher the migraine disability score (using the Migraine Disability Assessment Scale (MIDAS), that measures the impact of migraine attacks on daily life), the higher the risk of medication adaptation. Close to half (45%) of people with severe disability reported acute medication overuse in the last month, compared with only 1% of those with mild disability. Of all those who reported overuse, 82% had severe disability.
When we looked at the types of acute medication that were being used more often than recommended in the last month, triptans were most commonly used. Overall, 30% of respondents used triptans on 10 days or more in the last month. This is probably because triptans can be very effective, more so than paracetamol or opioids, and we want to take the most effective medication to treat a migraine attack. However, although opioids aren’t recommended at all for the treatment of migraine because of the risk of dependency and side effects (as well as medication adaptation headache), they were being over-used in nearly 20% of respondents and half of those with chronic migraine.
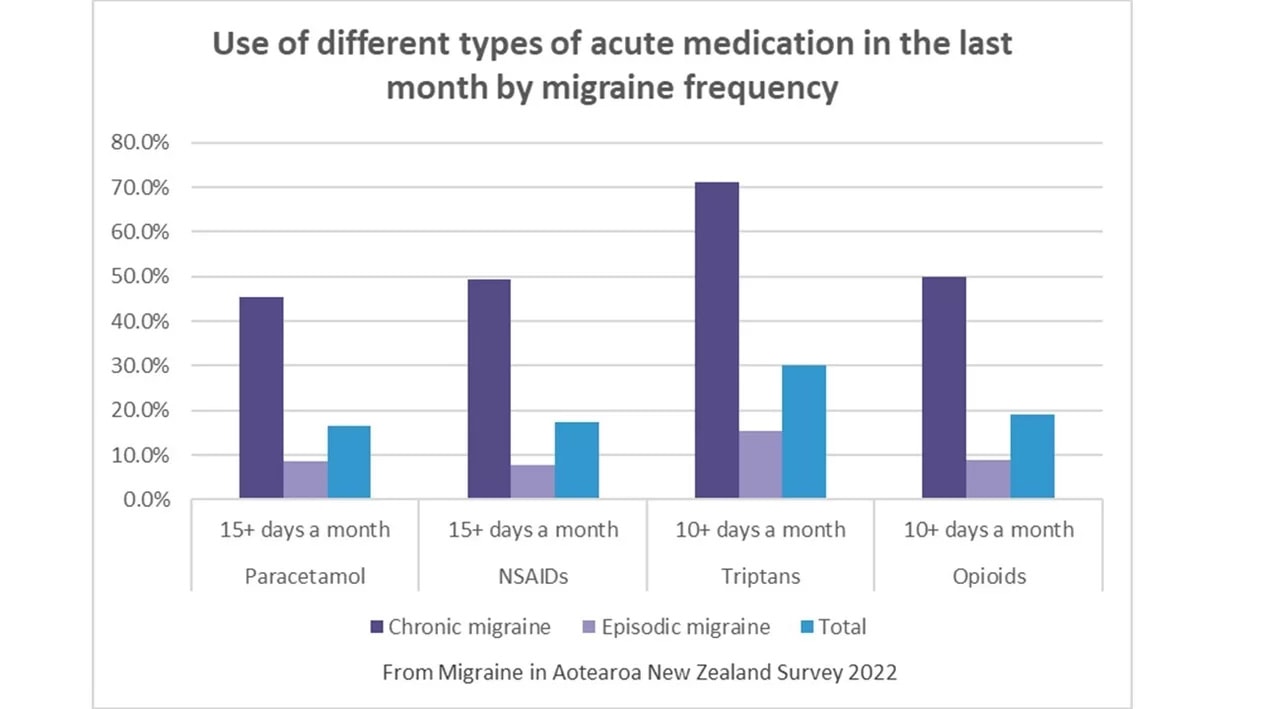
This highlights, more than anything, the critical need for more acute medication options, that are safe, effective and affordable. Access to a wider range of triptans (we only have two options in New Zealand) and to new treatments now available overseas (e.g. the ditan lasmiditan/Reyvow and gepants such as rimegepant/Nurtec and ubrogepant/Ubrelvy) would mean more people could effectively treat acute migraine attacks – and potentially fewer people would develop chronic migraine. As an added bonus, the new gepant class of medication does not appear to create any risk of medication adaptation headache.
Survey respondents specifically asked for this, when we asked them what could be done to improve their life with migraine. They wanted medication that would “relieve migraine symptoms without the risk of overmedicating” and not have to worry about medication overuse. To all the gepants out there – New Zealand is waiting for you.


