Results from the Migraine in Aotearoa New Zealand Survey 2022
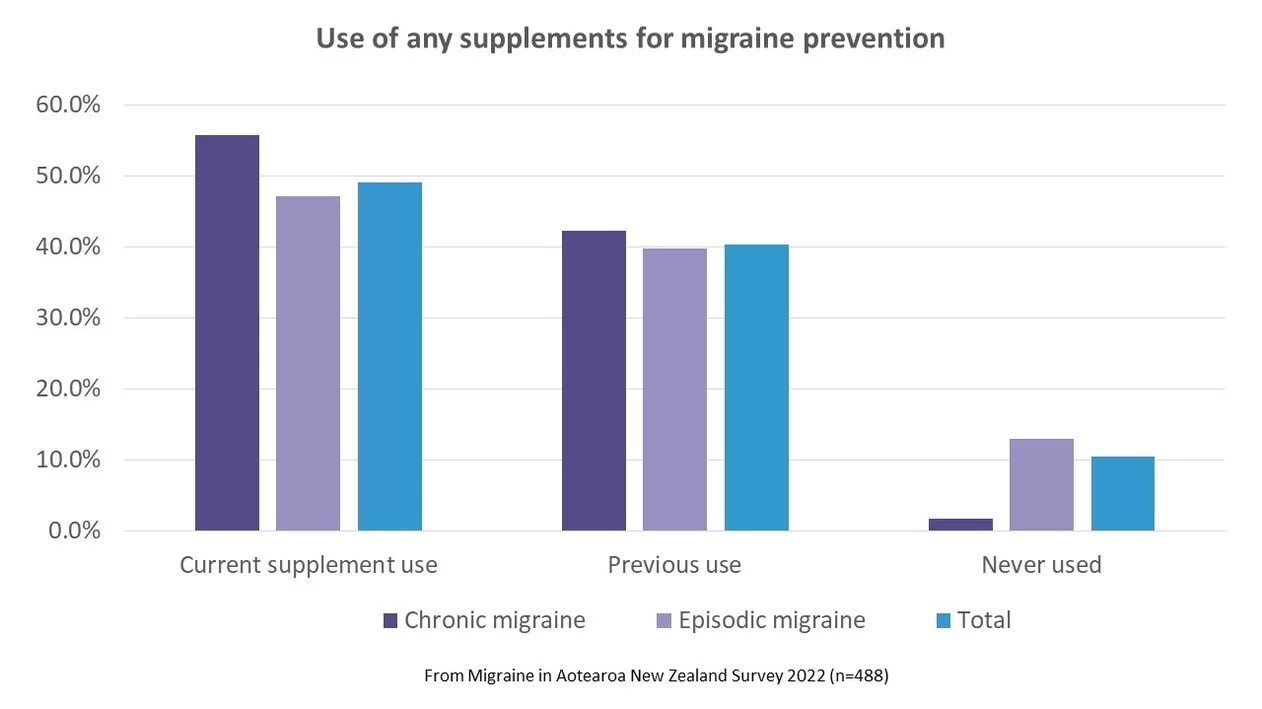
Many people with migraine take supplements – which encompasses vitamins, dietary and food supplements, and herbal remedies. In the Migraine in Aotearoa New Zealand 2022 Survey, almost half (49%) of participants were currently taking a supplement and 40% had previously used one. These proportions were a little higher for people with chronic migraine (headache on 15 days or more a month). Only 2% of people with chronic migraine had never used a supplement for migraine, compared with 13% of people with episodic migraine.
Supplement use for migraine prevention was about as common as prescribed medication (half of the survey respondents were taking medication for prevention). Many respondents were taking both – of those who were currently taking a supplement, 55% were also currently taking a prescribed preventive medication.
We asked specifically about supplements that are recommended in international guidelines and/or have at least some evidence for effectiveness in migraine prevention from clinical trials. ¹ These were magnesium, riboflavin (vitamin B2), coenzyme Q10, feverfew and butterbur.
Some of these supplements come with a note of caution. There have been concerns about potential liver toxicity with the use of butterbur and this has led some countries to withdraw this product from the market. Only formulations that are certified to contain the active ingredient, Petasites, and be free of liver toxins should be taken, and consultation with a doctor is advisable. It’s a good idea to ask your doctor about any type of supplement use, to check for possible interactions with other medications, or side effects, but this is particularly important for a supplement like butterbur. Feverfew is not recommended in pregnancy and the evidence for its effectiveness is weak.²
The supplements commonly being used by survey respondents were magnesium (42%) and riboflavin (22%). These were also the supplements that were most commonly used in the past but stopped for some reason (31% had previously used magnesium, 22% had previously used riboflavin). That still left a large proportion of people who had never tried these supplements but would like to (18% for magnesium, 39% for riboflavin).
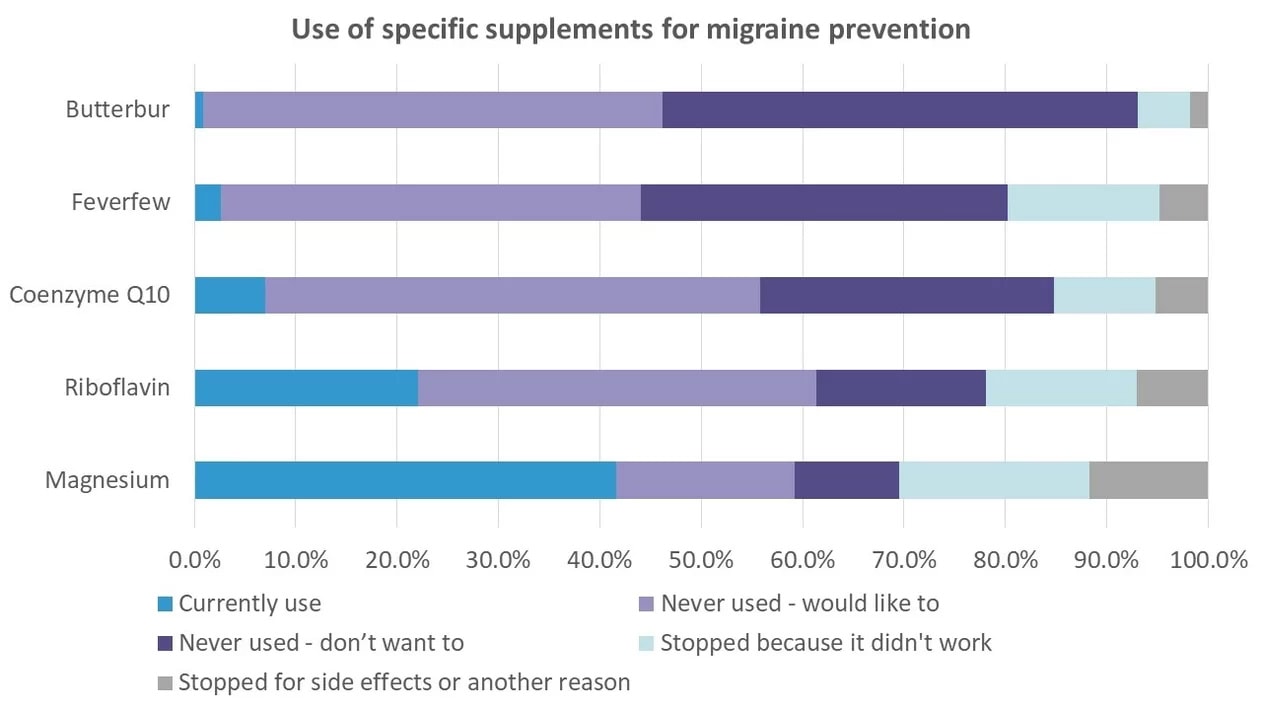
Few people were currently using coenzyme Q10, feverfew or butterbur. A higher proportion had used them in the past but stopped (15% for coenzyme Q10, 20% for feverfew and 7% for butterbur). Close to half of respondents would like to try one or more of these supplements (49% for coenzyme Q10, 41% for feverfew and 45% for butterbur).
For all supplements, by far the most common reason for stopping them was because they didn’t work. Stopping because of side effects was much less frequent. For example, 16% of respondents had previously used magnesium but stopped because it didn’t work, but only 5% had previously used and stopped because of side effects. Supplements can cause side effects, but these are often milder than for prescription medications and less disturbing (bright yellow urine from riboflavin is not nearly as strange as the burning, tingling toes from topiramate). Although we didn’t ask people to specify the ‘other reasons’ why they discontinued supplements, cost and access are likely causes.
For people currently taking supplements, just over half (52%) were taking only one, 38% were taking two and 11% were taking between three and five supplements.
Survey respondents also mentioned other supplements they were using. There’s some promising evidence for omega 3 and vitamin D3 in the treatment of migraine; iron may reduce migraine attacks in people with iron deficiency; and there are anecdotal reports that ginger, although usually used as an acute remedy, may be helpful if consumed daily. Melatonin is also often considered a supplement but isn’t readily available without a prescription in New Zealand, so this is discussed in another article on prescription hormones (melatonin is also considered a hormone).
What can we say about supplement use from the survey? Supplements were widely used but they didn’t work for everyone. They were often used in combination with medication. The commonly used supplements were the ones with the best evidence and safety profiles (magnesium and riboflavin). There were a lot of people who would like to try them but hadn’t – maybe because of cost, accessibility or lack of information. They can be expensive and not all pharmacies will stock the doses that are specific for migraine treatment.
It’s yet another confirmation of what we know – the treatments for migraine available in New Zealand are not sufficient. Some treatments work for some but not for all. We need more options and we need more research into alternatives, including other supplements. The more choices we have in the toolkit, the better for everyone.
Further reading
- Migraine supplements – the big 5 you should know about, Migraine Strong
- Evidence-based integrative treatments for headache
- Supplements, The Migraine Trust
References
- Kuruvilla, D. and Wells, R.E. (2019), Evidence-Based Integrative Treatments for Headache. Headache: The Journal of Head and Face Pain, 59: 971-972. https://doi.org/10.1111/head.13555
- Wider B, Pittler MH, Ernst E. Feverfew for preventing migraine. Cochrane Database Syst Rev. 2015 Apr 20;4(4):CD002286


