Results from the Migraine in Aotearoa New Zealand Survey 2022
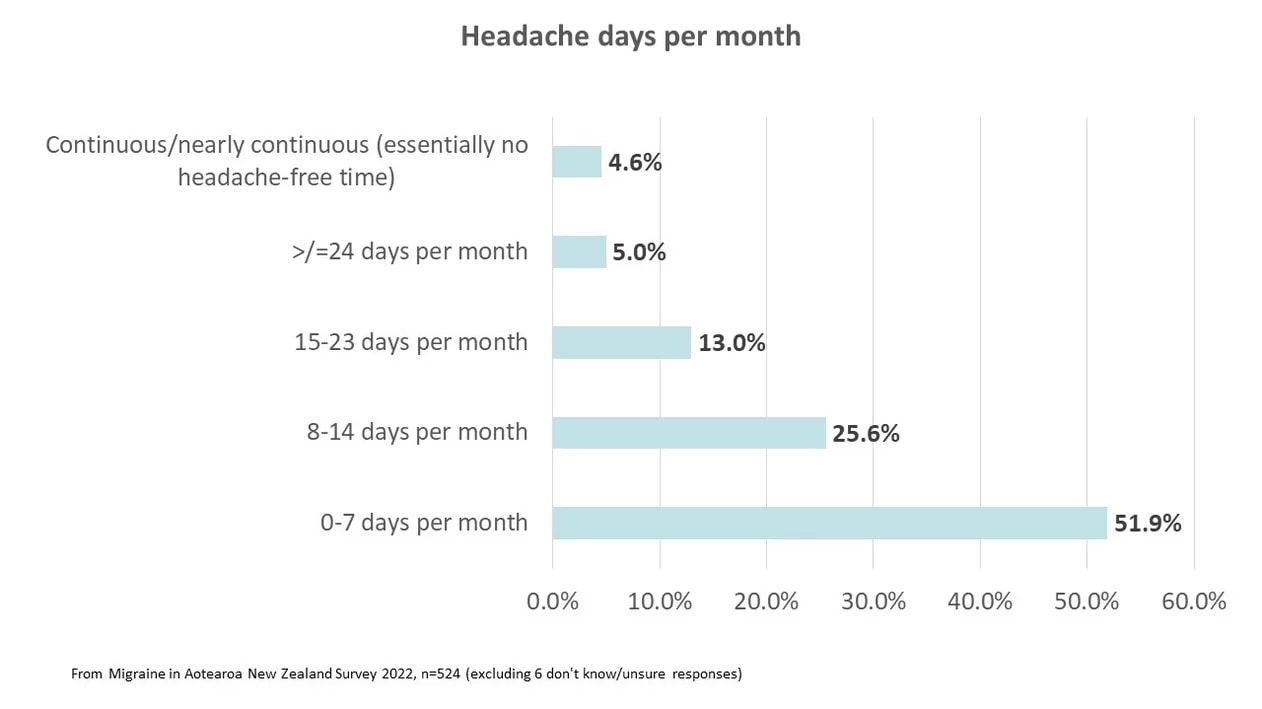
One of the most annoying aspects of a migraine attack is that it can be unpredictable and random, coming on without any warning, and disrupting plans for the day, whether these were for work, socialising or getting through a list of chores. But what is even worse is when migraine attacks come so frequently they’re almost predictable. This is the difference between episodic migraine (attacks occurring on up to 14 days a month) and chronic migraine (headache on 15 days or more a month for at least 3 months), although the disruption to the life of someone with high-frequency episodic migraine (8-14 days a month) can be similar to chronic migraine.
Estimates for the prevalence of chronic migraine vary but is probably in the range of 1-2% of the population.¹ Chronic migraine usually develops from episodic migraine, with around 3% of people with episodic migraine transforming to chronic migraine per year.² Chronic migraines can also revert back to episodic (one study found that 26% of people with chronic migraines reverted to episodic migraines after two years).³ Chronic migraine can be prevented or reverted with effective treatment of acute attacks, avoidance of overuse of acute medications and early use of effective preventive medication.⁴
In the 2022 Migraine in Aotearoa New Zealand Survey, 22% of respondents had chronic migraine (15 or more headache days a month).
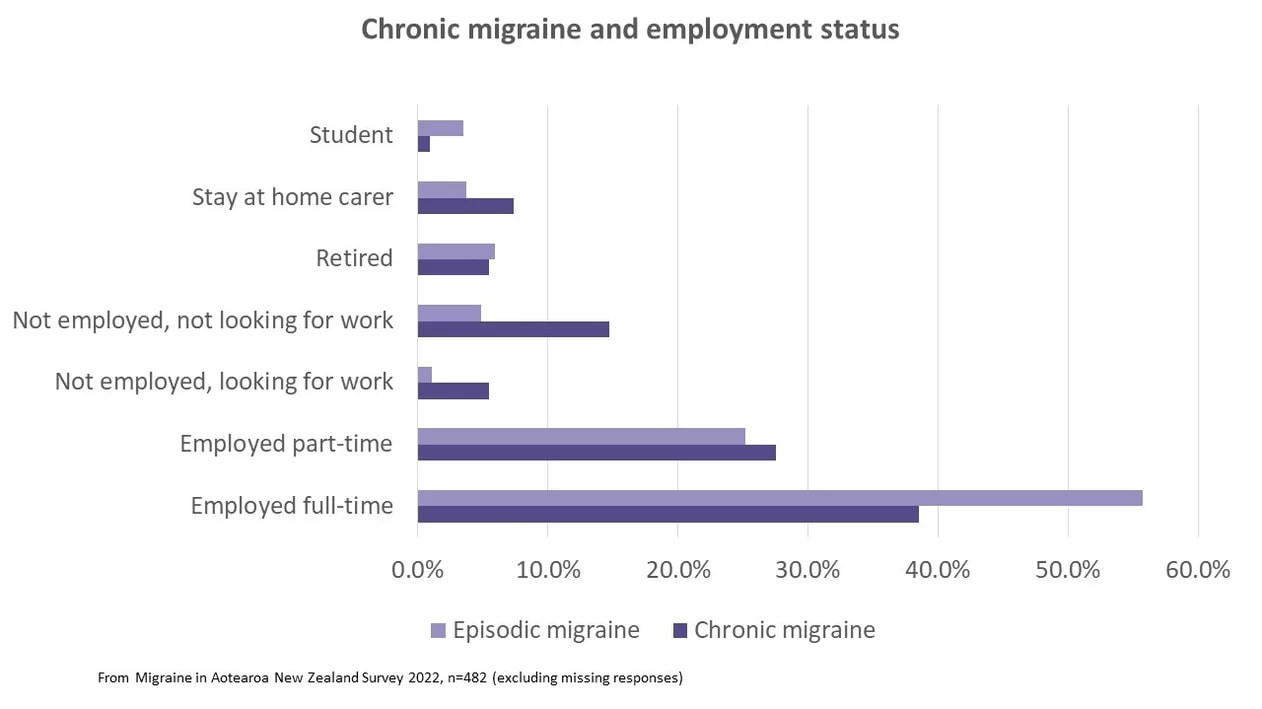
From the survey, the presence of chronic migraines had an impact on employment, with fewer people with chronic migraines working full-time, compared to those with episodic migraines, and more people with chronic migraines being unemployed and not looking for work.
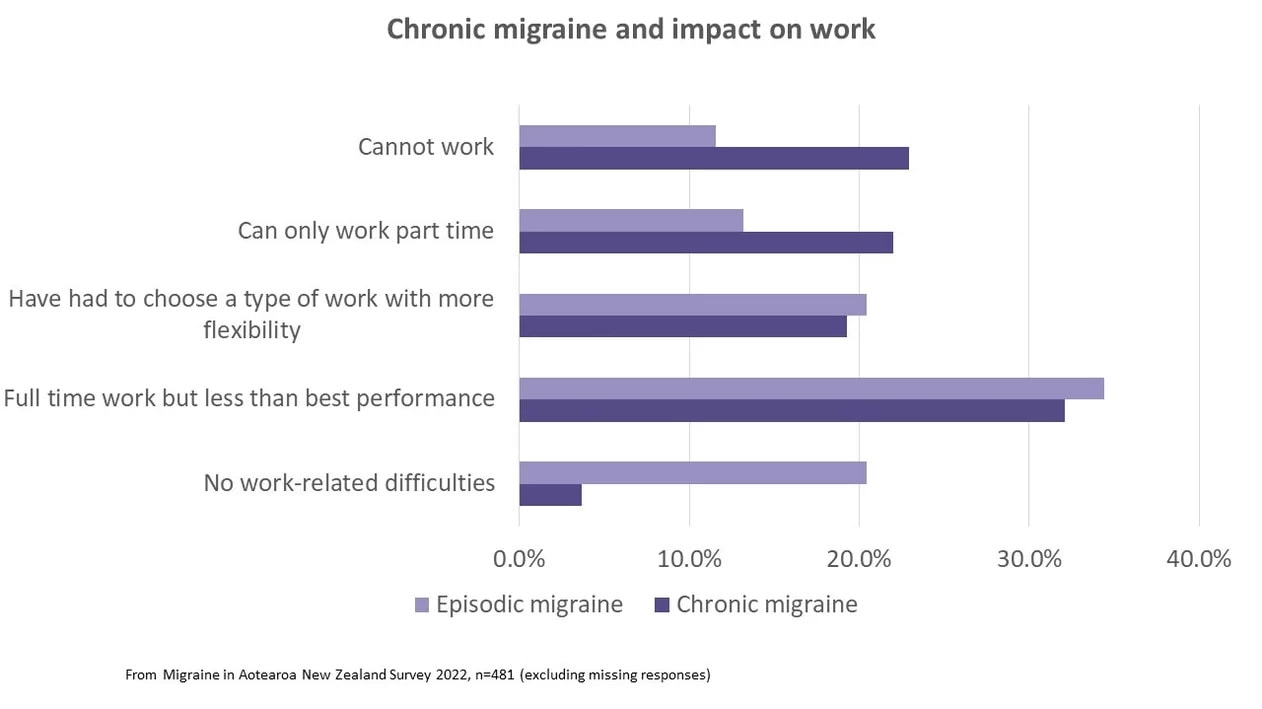
Similarly, when we asked respondents what impact migraines had on their ability to work, people with chronic migraines were much less likely to report having no work-related difficulties and more likely to be unable to work or working part-time than those with episodic migraines.
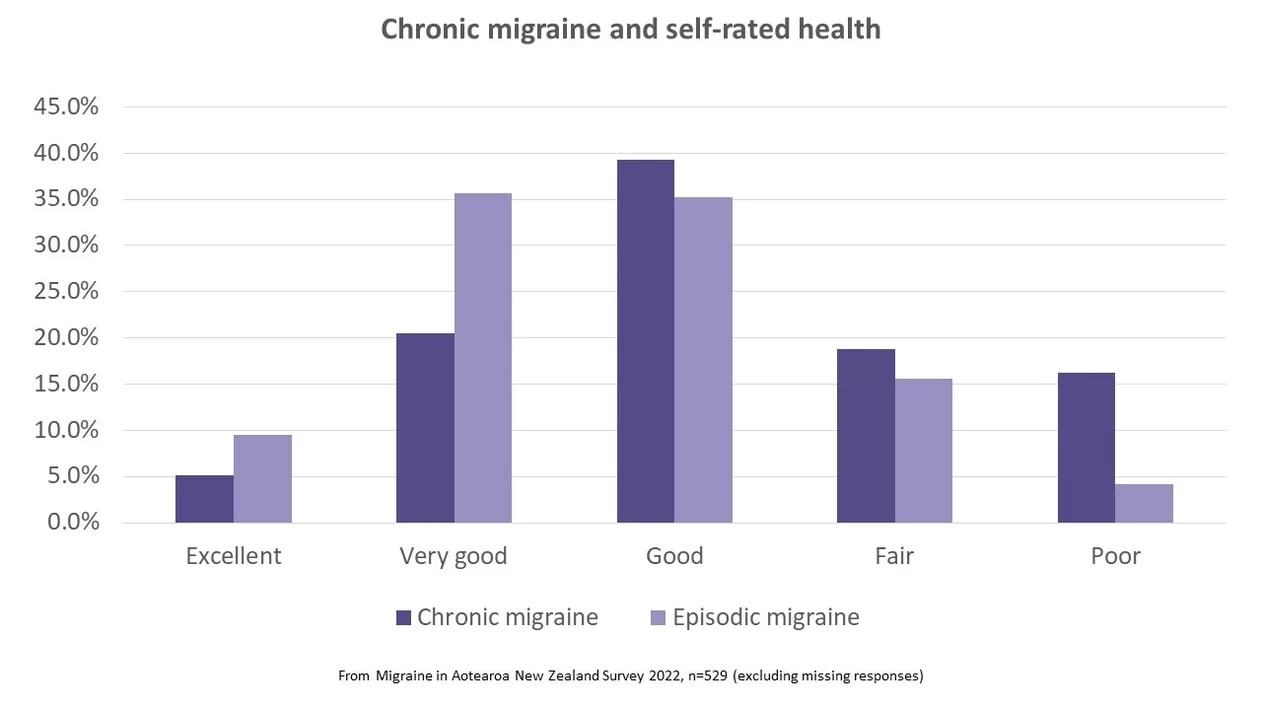
Chronic migraine also affects how people feel about their health. Over a third (35%) of respondents with chronic migraine assessed their health as ‘fair’ or ‘poor’ (compared to 20% of those with episodic migraine). From national surveys,⁵ over 90% of people in New Zealand rate their health as excellent, very good or good. From this survey, all people with migraine are faring much worse than the general population in their experience of health.
The burden of migraine, and particularly chronic migraine, is clearly shown in these results. One of the survey respondents summed it up in these words:
“As a single parent, losing work days to migraines causes financial strain and low mood due to feeling inadequate and unreliable to my colleagues. The toll migraine headaches take on a person’s mental health is devastating and severely overlooked. You feel useless and worthless because you can’t provide. Even completing daily household tasks can be challenging when you feel so unwell. It’s very isolating when you have chronic migraines that keep you shut away in the dark and in silence. Your self-worth takes a dive.” (Māori female, aged 35-44 years)
Chronic migraine can take an enormous toll and more needs to be done, to support people with chronic migraines, those that depend on them and those that care for them. It’s 2023 and an election is looming. This is the time to listen to what the politicians are promising and ask searching questions – who is committed to funding the medications and health services that we and others with health issues need access to? Who will ensure workplaces and employers are willing and able to provide flexibility and accommodations to people with migraines? Who will speak out against the stigma of diseases like migraine which are poorly understood and often trivialised? Who will pledge to increase migraine research in New Zealand?
References
- Burch, R. C., Buse, D. C., & Lipton, R. B. (2019). Migraine: Epidemiology, Burden, and Comorbidity. Neurologic Clinics, 37(4), 631–649; Hovaguimian, A., & Roth, J. (2021). State of the art review: Management of chronic migraine. BMJ, 379(e067670)
- May, A., & Schulte, L. H. (2016). Chronic migraine: Risk factors, mechanisms and treatment. In Nature Reviews Neurology (Vol. 12, Issue 8, pp. 455–464)
- Manack, A. N., Buse, D. C., & Lipton, R. B. (2011). Chronic migraine: epidemiology and disease burden. Current Pain and Headache Reports, 15(1), 70–78.
- Ferrari, A., Baraldi, C., & Sternieri, E. (2015). Medication overuse and chronic migraine: a critical review according to clinical pharmacology. Expert Opinion on Drug Metabolism & Toxicology, 11(7), 1127–1144; Manack, A. N., Buse, D. C., & Lipton, R. B. (2011). Chronic migraine: epidemiology and disease burden. Current Pain and Headache Reports, 15(1), 70–78; May, A., & Schulte, L. H. (2016). Chronic migraine: Risk factors, mechanisms and treatment. In Nature Reviews Neurology (Vol. 12, Issue 8, pp. 455–464).
- https://socialreport.msd.govt.nz/health/self-rated-health.html