Results from the Migraine in Aotearoa New Zealand Survey 2022
There are many reasons to treat a migraine attack – not only to avert the pain and disability of the attack but also because inadequate treatment of acute attacks can lead to more frequent attacks.¹ The nervous system can become more sensitised to pain with repeated attacks to the point where even a minor stimulus provokes a severe response.²
Unfortunately, not everyone treats migraine attacks adequately. Some people with migraine might only take over-the-counter medication such as paracetamol or non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or Voltaren and not realise migraine-specific acute treatments are available on prescription (the triptans). Some people with migraine don’t get prescribed triptans by their doctor, maybe because the doctor has failed to diagnose migraine correctly or isn’t familiar with current migraine treatments. Not everyone receives advice on ways to help the treatment work better, like taking a medicine for nausea (an anti-emetic) so drugs get absorbed more effectively.
But even if you take all the advice and all the appropriate medicine, it doesn’t always work. From a review of migraine medications, triptans relieved headaches within two hours in 42–76% of people; NSAIDs and paracetamol relieved headaches within two hours in 46–52% of people, which left a lot of people without adequate pain relief.³ In addition, NSAIDs have gastrointestinal and cardiovascular side effects and triptans are unsuitable for patients with cardiovascular disease so there can be limited treatment options for many people.⁴
In the Migraine in Aotearoa New Zealand Survey 2022, we asked respondents what medications they were currently using to treat migraine attacks, and what they had previously used but stopped because of side effects, lack of effectiveness or other reasons.
NSAIDs were the most popular currently used medications (61%), followed by caffeine (55%), triptans (55%) and paracetamol (49%). Few people had never used Paracetamol (3%) or NSAIDs (5%). Almost everyone who had previously used paracetamol had stopped because it didn’t work; for NSAIDs, there was a higher proportion who stopped because of side effects (7% of all respondents).
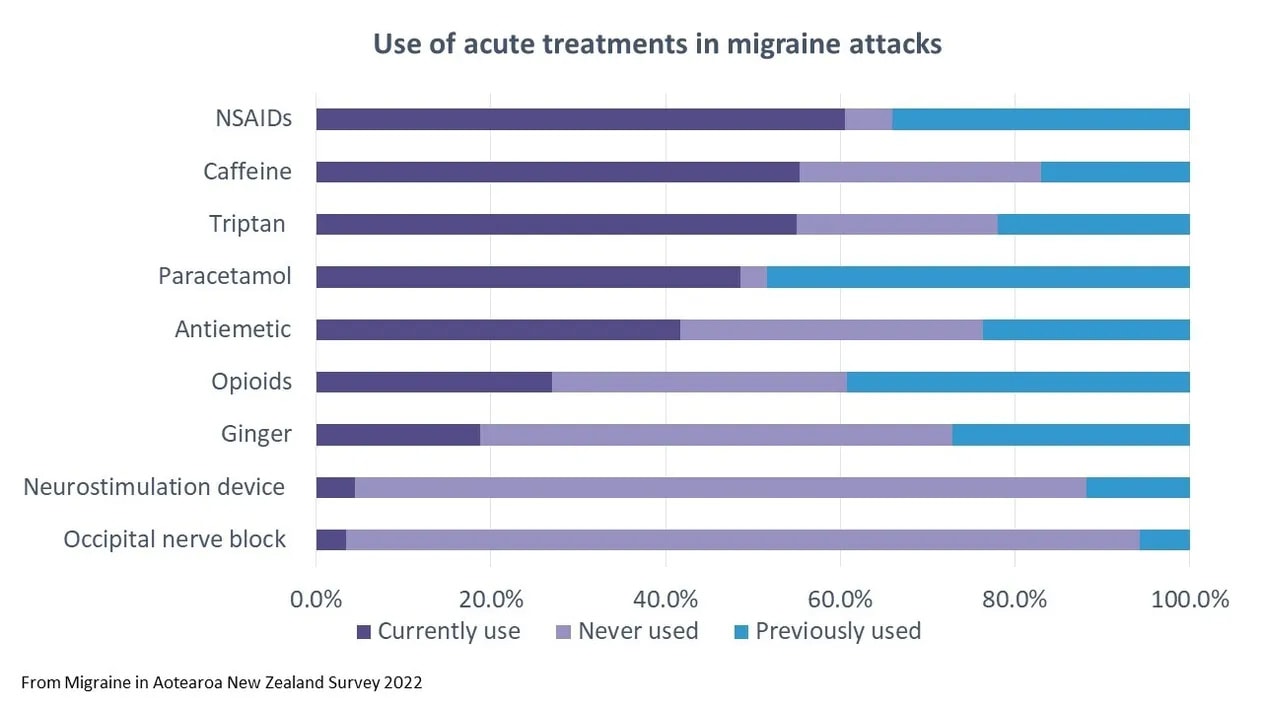
A similar proportion of people had used and stopped triptans because of side effects (9% for sumatriptan and 7% for rizatriptan) but a significant minority had never tried one or other of the triptans and would like to (25% for sumatriptan and 19% for rizatriptan). And although few people were using a neurostimulation device or occipital nerve block, around half of respondents would like to try these. This suggests there are barriers in the health system to accessing migraine-specific acute treatment – there’s demand for different treatment options that isn’t being met.
There’s also some possible mis-treatment – more than a quarter of respondents were taking opioids for migraine attacks, even though this isn’t a recommended treatment. This likely reflects the number of people who haven’t had success, haven’t been offered or can’t access other treatment options.
New types of drugs to treat migraine attacks are available in other countries (for e.g. gepants), and more are being developed and researched. We remain hopeful that in the near future we’ll have more options and choice in NZ for how we treat migraine attacks.
References
- Lipton, R. B. et al. Ineffective acute treatment of episodic migraine is associated with new-onset chronic migraine. Neurology 84, 688 (2015).
- Suzuki, K., Suzuki, S., Shiina, T., Kobayashi, S. & Hirata, K. Central Sensitization in Migraine: A Narrative Review. (2022) doi:10.2147/JPR.S329280.
- Cameron, C. et al. Triptans in the Acute Treatment of Migraine: A Systematic Review and Network Meta-Analysis. Headache: The Journal of Head and Face Pain 55, 221–235 (2015).
- Ailani, J., Burch, R. C. & Robbins, M. S. The American Headache Society Consensus Statement: Update on integrating new migraine treatments into clinical practice. Headache: The Journal of Head and Face Pain 61, 1021–1039 (2021).