Results from the Migraine in Aotearoa New Zealand Survey 2022
It’s been known for a long time that migraine disease tends to run in families. If you have a first-degree relative (parent, sibling or child) with migraine then your own risk of having migraine is 1.5 to four times higher than someone in the general population.¹ The risk is higher for relatives of people with migraine who have their first migraine attack before age 16 and those with very high pain scores.²
It’s complicated though. Genetics play only one part in the origin of migraine and in most people it’s due to an interaction between genes, the environment and probably other factors we’ve yet to identify. There are some rare cases of migraine that are due to particular genes, such as familial hemiplegic migraine, but for most people with migraine, there are many genes involved. So far, researchers have identified nearly 200 gene variants that are linked to molecular changes that could contribute to an increased migraine risk.¹ Most of these genes have code related to the central nervous system or the vascular system, which we know are involved in migraine attacks.
Genetic studies have also shown a shared genetic link between migraine and other health conditions, including depression, anxiety, insomnia, endometriosis, asthma, stroke, high blood pressure and irritable bowel disease.
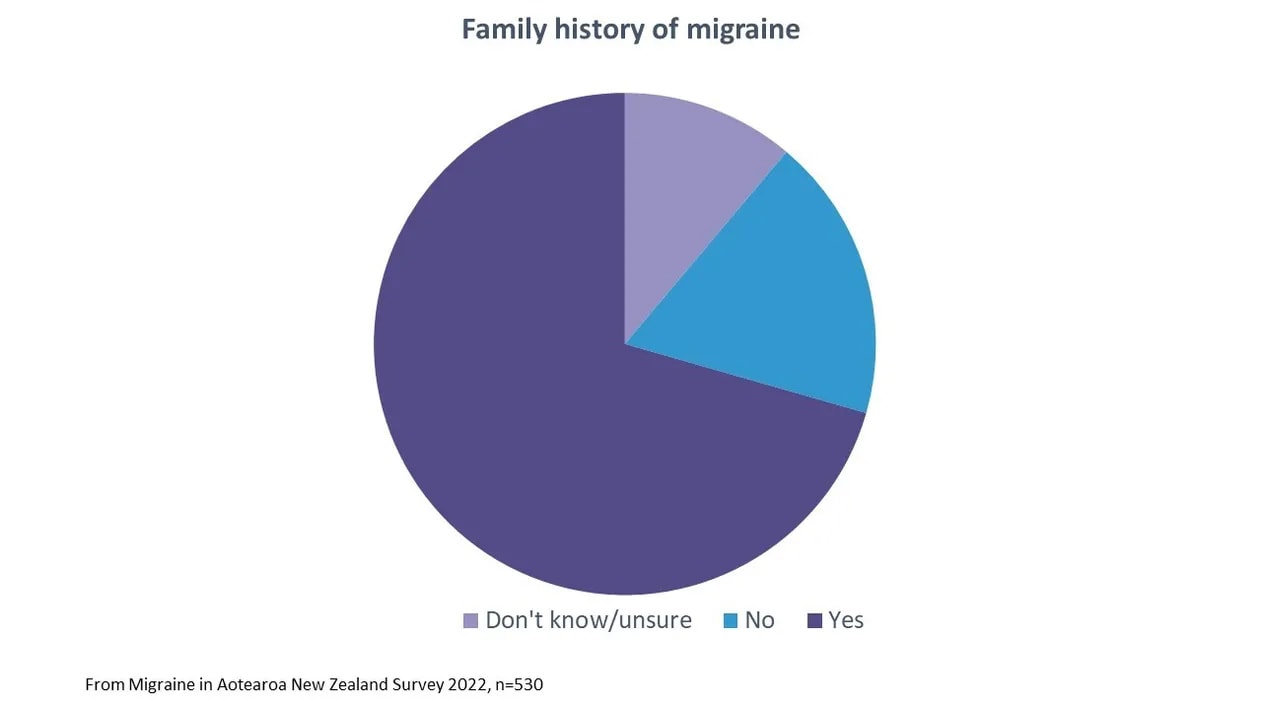
From the Migraine in Aotearoa New Zealand Survey 2022, 71% of people reported a family history of migraine. We asked whether ‘anyone else in your family’ had a migraine, so this could include more than first-degree relatives (e.g. grandparents, aunts and uncles). About one in ten people weren’t sure or didn’t know.
One advantage of having a family member with a migraine is that you may be able to recognise the issue earlier and get a diagnosis more quickly. You may be able to learn how to manage attacks and get more support. From the survey, respondents who had a family history of migraine reported feeling judged or misunderstood because of migraine from family a little less often (15%) than those without a family history (21%) or those who were unsure (20%). Clearly, a family history is not completely protective of feeling stigmatised because of migraine by family members.
There’s still work to be done to raise awareness of the impact and meaning of migraine disease, even with those closest to us.
References
- Grangeon, L. et al. Genetics of migraine: where are we now? Journal of Headache and Pain vol. 24 Preprint at https://doi.org/10.1186/s10194-023-01547-8 (2023).
- Stewart, W. F. et al. Familial risk of migraine. Neurology 66, 344–348 (2006).


