Results from the Migraine in Aotearoa New Zealand Survey 2022
In other Migraine in Aotearoa New Zealand Survey 2022 key insight reports, we’ve looked at how many people were taking prescription medication to prevent migraine, as well as supplements, hormones, injections and non-medication approaches.
We’ve noted the downsides of many of the older, non-specific preventive medications – their slow onset of action, inadequate effectiveness and intolerable side effects.¹ These downsides mean many people don’t stay on the medications and may have to try several different types of medication before they find one that works. These medications can also stop working over time.
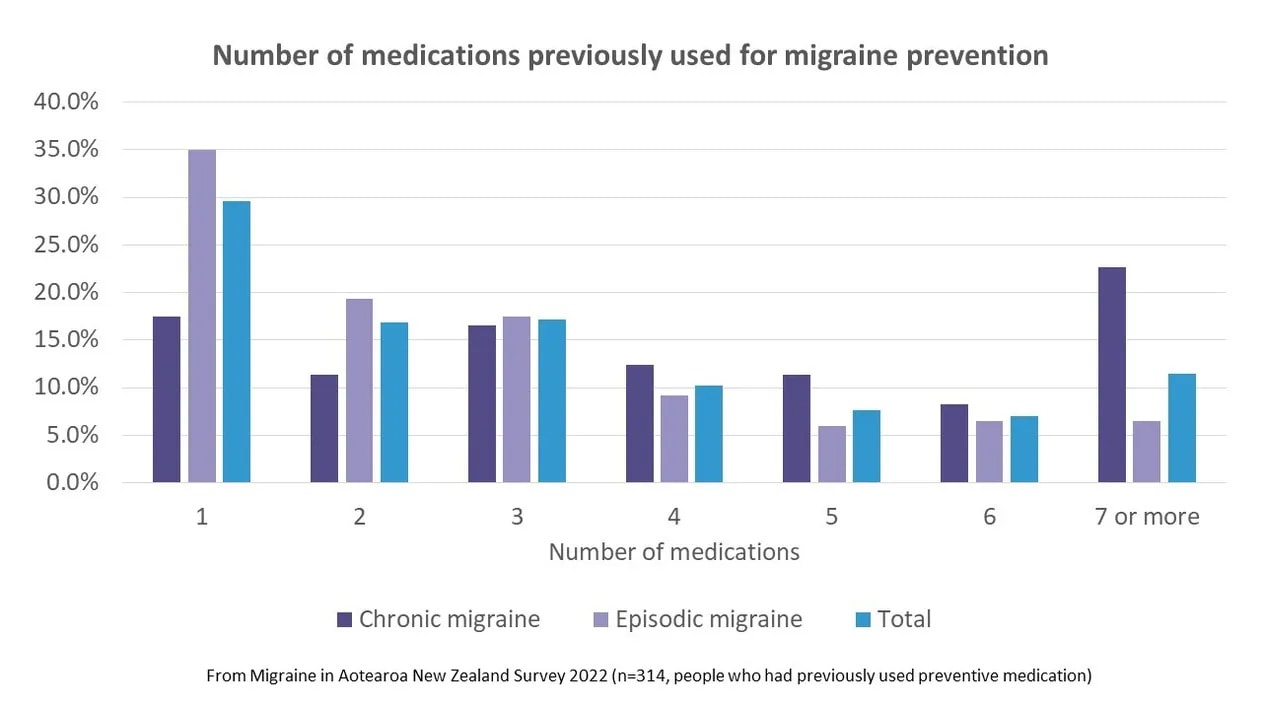
To investigate this further, we analysed how many prescribed oral medications people said they’d previously used or were currently using, for migraine prevention. This included all the specific medications asked about in the survey by name (antidepressants, antiepileptics, antihypertensives, pizotifen and melatonin) but excluded female/male hormones, botox and other injections and over-the-counter supplements. International research has found that among people with migraine who have ever used preventive medication, the average number used was four for people with chronic migraine and three for people with episodic migraine.²
In our survey, on average, people with chronic migraine* had previously used 3.6 medications for migraine prevention; people with episodic migraine had used an average of 1.5. This was for the whole sample, which included those who hadn’t previously used any preventive medications (47% of those with episodic migraine and 18% of those with chronic migraine). If we just looked at people who had previously used one of these medications, the average number of medications used was 4.4 for people with chronic migraine and 2.9 for people with episodic migraine – very similar to what has been found in other countries. People with chronic migraine were more likely to have tried seven or more preventive medications.
The maximum number of medications previously used was 18, but this was an outlier – the next highest number of medications previously used was 13.
We also looked at the number of medications people were currently taking for migraine prevention. Most (73% overall) were taking only one, but a higher proportion of people with chronic migraine were taking two or more (38% compared to 22% of those with episodic migraine). Overall, 27% of people taking preventive medication were taking two or more medications.
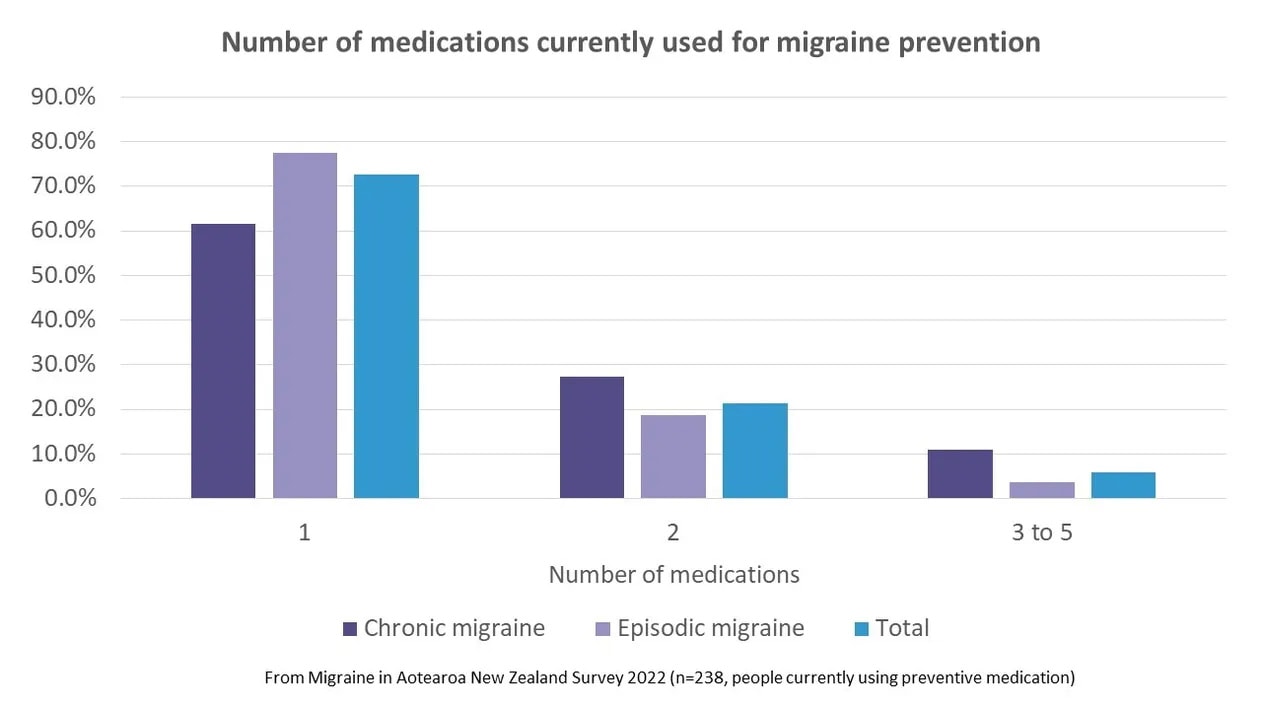
It’s common practice to add on another preventive medication when the first one hasn’t worked as well as the patient or clinician would like or perhaps has stopped working as well as it did initially. The fact that over a quarter of people taking preventives have found themselves in the position that they had to take another drug, and some even a third (or a fourth, or fifth…) is disturbing. Add this to the fact that so many people had tried and stopped taking preventives in the past (mostly because they didn’t work or because of side effects), a picture emerges of truly deficient preventive medication options.
This is why many people would like to try one of the newer migraine-specific medications targeting the brain peptide calcitonin gene-related peptide (CGRP). They don’t work for everyone, but they often act quickly, have few side effects and their effectiveness seems to be sustained.
This is why we should be asking any politician who is after our vote in 2023 what they’re going to do about access to and funding of new medications.
And this is why we (Migraine Foundation) exist – to advocate for better treatments, better services, more research and more awareness of the impact of migraine disease on so many New Zealanders. Please support our work by donating or becoming a member and spread the word through your family, friends, networks and social media.
*Defined as headache for 15 days or more per month for at least three months, with at least eight headache days a month characteristic of migraine; episodic migraine is defined as migraine occurring on up to 14 days a month.
References
- Ashina, M. et al. Migraine: integrated approaches to clinical management and emerging treatments. Lancet 397, 1505–1518 (2021).
- Blumenfeld, A. M. et al. Patterns of Use and Reasons for Discontinuation of Prophylactic Medications for Episodic Migraine and Chronic Migraine: Results From the Second International Burden of Migraine Study (IBMS-II). Headache: The Journal of Head and Face Pain 53, 644–655 (2013).


